Biométrie oculaire, calcul d’implant
Biométrie : définition
La biométrie oculaire est un examen qui permet le recueil de certaines dimensions de l’œil comme sa longueur axiale, afin de calculer la puissance de l’implant destiné à remplacer le cristallin au cours de la chirurgie de la cataracte. Rappelons que pour que la l’image rétinienne (et donc la vision) soit nette spontanément (sans correction lunettes ou lentilles), il faut que la cornée et l’implant posé après retrait de la cataracte focalisent la lumière incidente émise par la source lumineuse observée dans le plan de la rétine.
Quand on opère la cataracte, on ne modifie pas significativement la puissance optique (vergence) de la cornée. En revanche, le retrait du cristallin opacifié modifiée la réfraction (les propriétés optiques de l’oeil). On remplace le cristallin opacifié par un implant dont la puissance optique est choisie pour induire la réfraction désirée en postopératoire: vision nette de loin sans lunettes (emmétropie), vision nette de près sans lunettes (myopisation légère). L’implant peut être monofocal+/- torique, multifocal+/- torique.
La biométrie oculaire vise à recueillir les données permettant de calculer (prédire) la puissance de l’implant (vergence) qui, combinée à celle de la cornée, permettra à l’oeil d’être corrigé pour la distance de vision nette sans lunettes souhaitée. La biométrie oculaire regroupe donc le recueil de données biométriques (longueur axiale, mesure de la puissance cornéenne= kératomérie, etc.), et permet la prédiction de la puissance optique de l’implant destinée à obtenir la réfraction postopératoire de l’oeil opéré.
En savoir plus: D Gatinel Calcul de puissance d’implant en chirurgie cataracte REALITES OPHTALMOLOGIQUES-Mai 2023-2
Une section de ce site est entièrement consacrée aux fondamentaux du calcul biométrique pour établir la puissance des implants en chirurgie de la cataracte (en anglais).
(voir également: formule de calcul PEARL-DGS, proposée par les Dr Debellemanière, Gatinel et Saad et qui repose sur l’intégration de données biométriques par un algorithme d’intelligence artificielle: https://iolsolver.com/
En plus de la longueur de l’oeil (longueur axiale) qui est aujourd’hui mesurée par une technique d’interférométrie, la biométrie oculaire nécessite la mesure d’autres paramètres oculaires comme la puissance optique de la cornée (kératométrie), la profondeur de la chambre antérieure (distance entre cornée et cristallin), diamètre cornéen, épaisseur du cristallin, etc. (voir :calcul de la puissance de l’implant dans un oeil modèle simplifié). La prédiction de cette puissance, qui permettra par exemple à l’œil de voir net de loin sans lunettes (emmétropisation), fait appel à une formule dite formule de calcul de la puissance de l’implant (il existe plusieurs types de formules pour le calcul de l’implant, et certaines sont plus précises que d’autres selon la morphologie initiale de l’œil considéré). En cas d’astigmatisme cornéen (un astigmatisme interne disparait avec le retrait du cristallin lors de la chirurgie), on peut envisager la pose d’un implant dit « torique« , et ceci nécessite un calcul supplémentaire (pour déterminer l’axe et le degré de correction de l’astigmatisme apporté par l’implant).
Pourquoi doit-on faire une biométrie avant chirurgie de la cataracte?
La pose d’un implant de cristallin artificiel est de rigueur au cours de la chirurgie de la cataracte, où le cristallin est retiré (son enveloppe, le sac capsulaire, est préservé et sert de support anatomique pour l’implant). Le cristallin est une lentille dont le pouvoir optique est (avant la survenue de la cataracte) généralement voisin de 22 Dioptries : couplé à la cornée, le cristallin agit comme un lentille convergente qui permet de focaliser les rayons lumineux dans le plan de la rétine. Le retirer laisse l’oeil dans un état dit d' »aphakie » (oeil aphake). Du fait de la perte de la vergence (puissance optique) du cristallin, l’oeil aphake présente un important défaut de puissance (hypermétropie forte).
Un dialogue préliminaire est nécessaire avec le patient pour choisir la stratégie de correction visuelle. La plupart des patients opérés de cataracte souhaitent rester ou devenir emmétropes (bénéficier d’une bonne vision de loin non corrigée après l’intervention). Certains patients, initialement myopes, souhaitent le rester pour pouvoir lire sans lunettes (s’ils sont très myopes, une réduction partielle de la myopie est indiquée pour laisser une myopie résiduelle proche de -2.50 à 3 D). L’avènement des implants multifocaux impose une biométrie précise: les implants multifocaux doivent permettre une correction optimale de la vision de loin, pour que l’addition qu’ils possèdent pour la vision de près soit efficace et que le patient puisse devenir indépendant aux lunettes en post opératoire.
On pourrait imaginer qu’il pourrait être intérssant de mesurer la puissance du cristallin avant de le retirer et le remplacer par un implant de même puissance. Cependant, il n’est pas facile de mesurer le pouvoir optique du cristallin in vivo; de plus, quand le patient présente une amétropie en préopératoire (myopie, hypermétropie, etc.), le remplacement du cristallin par un implant qui aurait la même puissance n’est pas intéressant. En effet, il laisserait l’oeil opéré et implanté (oeil dit « pseudo phake ») avec le même défaut optique qu’avant l’opération.
La biométrie vise à recueillir les éléments anatomiques permettant de calculer la puissance de l’implant de cristallin artificiel qui permettra à l’oeil opéré d’atteindre le statut réfractif souhaité (emmétropie, ou myopie légère). La vergence de la cornée alors ajoutée à celle de l’implant permettent à la lumière émise par une source lointaine d’être focalisée sur la rétine (emmétropie) ou légèrement en avant (myopie légère).
Correction lunettes préopératoire, postopératoire, et puissance d’implant
Correction lunette préopératoire et puissance d’implant
Une question fréquemment soulevée par les patients concerne le lien entre la puissance de l’implant et la correction préopératoire (réfraction de l’oeil avant l’intervention)
Il n’y a pas de lien direct entre la correction d’un patient en lunettes avant l’opération et la puissance de l’implant à poser, car pour un même degré de myopie ou d’hypermétropie, il existe en réalité des conformations oculaires variées. Par exemple, pour une même hypermétropie initiale (ex: +3D), l’implant à poser n’aura pas la même puissance pour un oeil dont l’hypermétropie est principalement liée à une faible longueur axiale, que pour un oeil dont l’hypermétropie est principalement liée à une cornée plate (faible puissance cornéenne).
La présence d’une cataracte est susceptible d’affecter la correction préopératoire (myopisation d’indice).
Il existe toutefois certaines tendances: les yeux myopes (plus longs) reçoivent des implants de puissance plus faible (ex : moins de 20 D) que les yeux hypermétropes. La puissance généralement nécessaire pour induire une emmétropie pour un oeil initialement emmétrope est généralement comprise entre 20.5 et 22.5 D. Les yeux fortements hypermétropes requièrent des implants de puissance supérieure à 27D, parfois au delà de 30D.
Correction lunette postopératoire et puissance d’implant
La biométrie est destinée à prédire la puissance de l’implant destinée à induire la correction souhaitée par le patient une fois l’implant inséré dans l’oeil après retrait du cristallin. Pour les mêmes raisons, il n’est pas possible d’établir une relation linéaire entre puissance à poser et correction lunette postopératoire. Il faut disposer des mesures de la puissance cornéenne, de la longueur de l’oeil, et d’une estimation précise de la position attendue de l’implant une fois inséré dans l’oeil.
Biométrie oculaire: paramètres du calcul de la puissance de l’implant
La biométrie permet de mesurer au moins deux paramètres indispensables:
– la longueur axiale : elle sépare le sommet de la cornée (vertex) de la rétine fovéale.
– la kératométrie: la mesure de la courbure de la cornée centrale (autour du vertex) permet de prédire la puissance optique de la cornée (vergence cornéenne).
Ces deux paramètres suffisent en théorie à déterminer la puissance de l’implant detiné à induire la correction réfractive souhaitée, à condition de connaître à l’avance la position précise de l’implant dans l’oeil opéré. Or, cette position ne peut être que prédite, et de faibles variations (ex: quelques centaines de micron) peuvent influer significativement sur la correction apportée par implant. Ceci explique que le calcul d’implant de soit pas une science exacte et expose à un certain degré d’imprécision! Dans ce contexte, la biométrie et le calcul d’implant ont une précision qui est d’auant plus élevée que l’oeil mesuré est un oeil « moyen », pour lequel la prédiction de la position de l’implant (fondée sur des modèles statistiques, avec un apport significatif de l’intelligence artificielle) sera plus juste. Ce point sera détaillé plus loin, mais il est important de bien réaliser qu’une formule de calcul comporte deux modules: un module optique et un module de prédiction de position de l’implant. (le second étant nécessaire pour utiliser le premier).
Les modèles statistisques destinés à prédire la position effective de l’implant requierent la mesure d’autres paramètres comme le diamètre cornéen, la distance initiale entre cornée et cristallin, l’épaisseur du cristallin, l’épaisseur de la cornée, etc.
Dans la plupart des cas, la mesure en elle- même est effectuée sans contact grâce à un biomètre optique non contact, qui utilise les propriétés de l’interféromètrie pour mesurer la longueur toale de l’oeil et de certains segments(ex: IOL Master, Zeiss, Anterion- Heidelberg Eng.). Le biomètre est également muni d’un kératomètre, et les systèmes plus récents (ex Anterionà) intègrent un système intégré de topographie cornéenne.
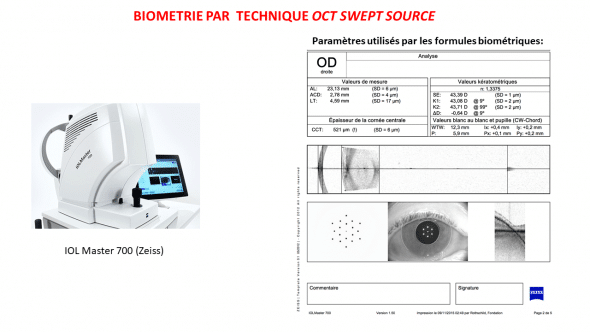
Paramètres biométriques recueillis avec l’instrument IOL Master 700 (technologie interférométrique couplée à swept source OCT)
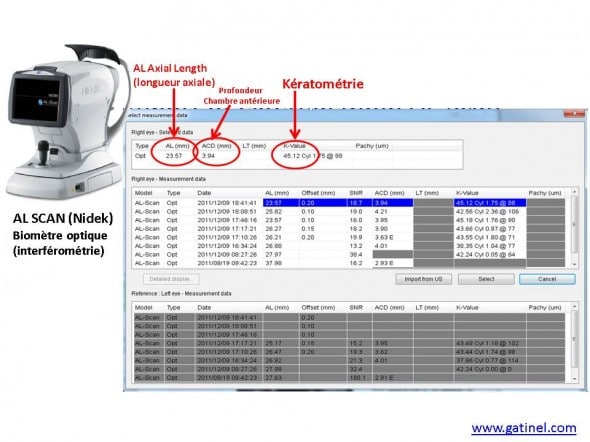
Représentation du biomètre AL SCAN (Nidek), qui dispose d’un système de mesure de la profondeur de la chambre antérieure par caméra Scheimpflug. Le logiciel du biomètre fait l’acquisition de la valeur de la longueur axiale, de la kératométrie, et de la profondeur de la chambre antérieure.
Il est important de remarquer que toute imprécision de mesure de l’un de ces paramètres aura un retentissement sur le calcul de la puissance de l’implant.
La figure suivante représente schématiquement les paramètres utiles au calcul optique:
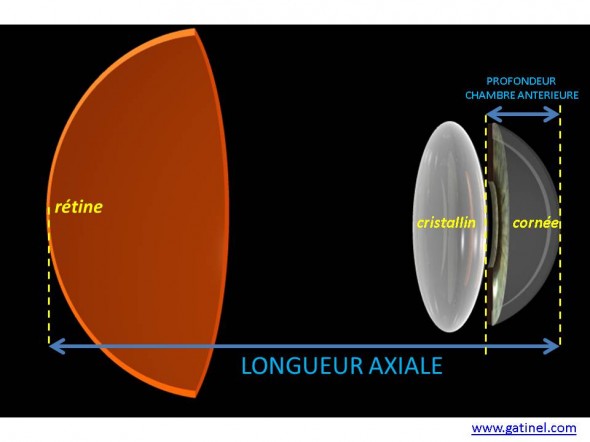
La longueur axiale représente la distance entre la rétine et le sommet de la cornée. Pour que la lumière soit focalisée sur la rétine, la cornée et le cristallin doivent faire converger les rayons incidents de manière à ce qu’ils soient focalisés en un point dans le plan de la rétine. La profondeur de la chambre antérieure correspond anatomiquement à l’écart entre le sommet de la cornée et le sommet de la face antérieure du cristallin. La puissance optique de la cornée est estimée grâce à la kératométrie.
En cas de cataracte avancée, la longueur axiale n’est pas modifiée, de même que la kératométrie. En revanche, la profondeur de la chambre antérieure peut être réduite, car le volume du cristallin augmente au fur et à mesure qu’il perd sa transparence. La profondeur de la chambre antérieure est modifiée en postopératoire (élargissement). Il existe une corrélation statistique entre profondeur de chambre antérieure et postérieure, qui justifie la mesure de ce paramètre en préopératoire.
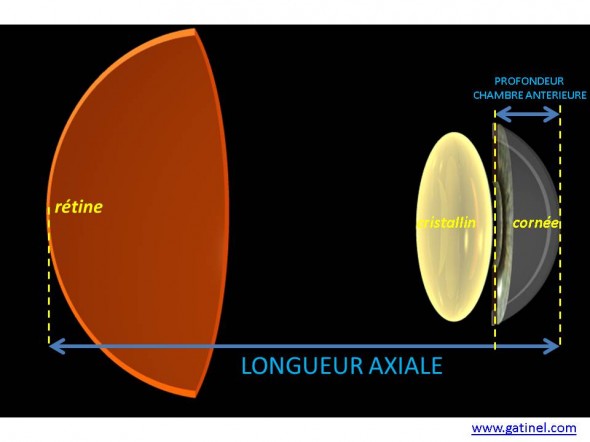
En cas de cataracte, l’épaisseur du cristallin augmente; ceci réduit la profondeur anatomique de la chambre antérieure.
Une fois le cristallin retiré, au cours de la chirurgie de la cataracte, l’oeil est « aphake« : sa réfraction est hypermétropique: la vergence de la cornée seule n’est pas suffisante pour faire converger la lumière sur la rétine (sauf en cas de longueur axiale très importante: myopie très forte).
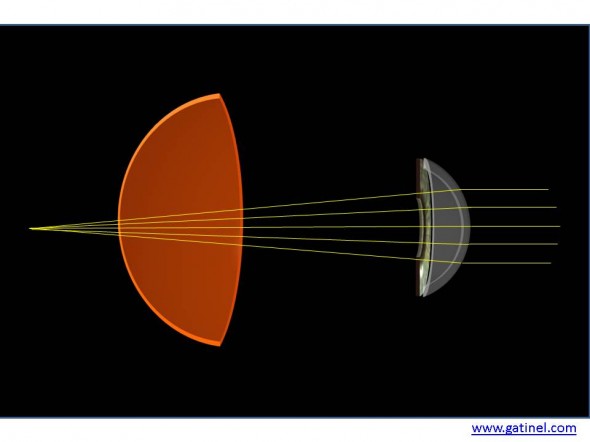
Après retrait du cristallin au cours de la chirurgie de la cataracte (le sac cristallinien qui est préservé n’est pas représenté ici), l’oeil est aphake et sa réfraction est généralement hypermétrope en l’absence de pose d’un implant. En effet, la vergence de la cornée est insuffisante pour focaliser la lumière émise par les sources observées sur la rétine (sauf si l’oeil est très long, c’est à dire atteint d’une myopie forte: dans certains cas de myopie extrêmes, la puissance de l’implant est alors proche de zéro, voire négative!).
Même si l’extraction du cristallin opacifié restaure la transparence des milieux oculaires, il est nécessaire pour des raisons optiques expliquées précédemment (réfraction postopératoire) de remplacer le cristallin par une lentille dont la vergence (puissance) doit être calculée en fonction des paramètres biométriques suivant :
– réfraction souhaitée: emmétropie (vision de loin nette sans lunettes) ou myopie légère (vision de près nette sans lunettes)
– longueur axiale (plus l’oeil est long, moindre est la puissance de l’implant, et inversement: les myopes reçoivent des implants de moindre puissance que les hypermétropes)
– kératométrie : plus la vergence de la cornée est élevée (faible courbure centrale), moindre est la puissance de l’implant (et inversement)
– position adoptée de l’implant dans l’oeil après la chirurgie, que l’on appelle aussi « effective lens position« .
Parmi ces variables, il en est une qui ne peut pas être mesurée avant l’intervention : il s’agit de la position effective de l »implant dans l’oeil (« effective lens position », ELP) ; cette position n’est pas la même que celle du cristallin retiré, et elle dépend de nombreux paramètres, que les études statistiques rétrospectives, idéalement réalisées sur un volume important de données (« big data ») peuvent aider à encadrer. Cest en partie pour cette raison que certaines formules biométriques font appel à l’intelligence artificielle: en nourrissant des modèles de « machine learning » (apprentissage supervisé) par un nombre suffisant d’observations (typiquement des examens biométriques qui ont été utilisés pour des opérations de la cataracte dont on connait le type d’implant posé et le résultat réfractif final), on peut « apprendre des erreurs biométriques passées » et les réduire par des techniques de régression, de réseau convolutionnel ou de forêt d’arbres aléatoires (ex : formule PEARL-DGS que nous avons conçue: www.iolsolver.com).
En plus des paramètres anatomiques initiaux comme la profondeur de la chambre antérieure ou l’épaisseur du cristallin, certaines des caractéristiques de l’implant peuvent influer sur la position de celui-ci (sa distance vis à vis de la cornée). Les implants possèdent une certaines épaisseur, qui varie avec la puissance optique, et le design choisi par le fabricants. Leur puissance optique est étiquetée selon des mesures standardisées (un implant de 22D produit un effet optique de 22D sur un oeil artificiel, mais une fois dans l’oeil, dont les milieux sont différents, cette puissance peut en réalité être plus ou moins élevée.
Pour cette raison, on utilise un ajustement linéaire de position en fonction du type d’implant posé qui dispose ainsi d’une « constante », prore à la formule de calcul utilisée. La « constante A », dont l’origine est liée aux premières formules empiriques de calcul biométrique, permet plus ou moins directement d’ajuster la valeur qui sépare l’erreur moyenne constatée pour un implant donné sur une série significative de patients pour lesquels on visait un résultat donné. Elle est déterminée statistiquement par une technique de régression linéaire, après recueil d’un nombre suffisant d’observation, et permet de « recentrer la distribution des erreurs réfractives sur zéro ». Cet ajustement repose sur un incrément constant de la position prédite de l’implant par la formule (avancer un implant vers la rétine= augmenter d’un incrément la position prédite de l’implant provoque une augmentation de la puissance prédite, et inversement).
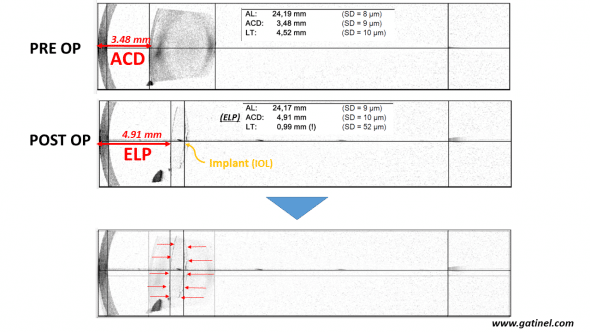
Biométrie optique (IOLMaster 700) avec coupe OCT swept source effectuée avant chirurgie de la cataracte (en haut) et après chirurgie de la cataracte avec pose d’un implant (au milieu). La position effective de l’implant (ELP) n’est pas connue avant la chirurgie, mais elle dépend statistiquement de certains paramètres qui sont utilisés dans les formules modernes de biométrie: profondeur anatomique de la chambre antérieure, épaisseur du cristallin, etc.
De cette incertitude sur la position finale de l’implant, découlent les enjeux des formules de calcul biométriques qui ont été successivement proposées, afin de mieux prédire la position dite effective de l’implant. C’est pour cela que le calcul biométrique est en partie fondé sur une conjecture; il repose sur le choix d’une position finale de l’implant dans l’oeil pour arrêter le calcul d’une puissance dioptrique destinée à fournir la réfraction souhaitée.
L’examen suivant, effectué avec un biométre interférométrique (IOLMaster 700, Zeiss) permet d’observer d’importantes différences biométriques entre les deux yeux d’un même patient qui présente une différence de réfraction entre les deux yeux (l’oeil droit est myope de -16 D; l’oeil gauche est myope de -8 D). La longueur axiale de l’oeil droit est largement supérieure à celle de l’oeil gauche. Cette élongation semble également concerner la profondeur de la chambre antérieure de l’oeil droit. En revanche, l’épaisseur du cristallin est sensiblement identique entre les deux yeux, de même que la kératométrie. La formule SRK T ne prend pas directement en compte la mesure de la profondeur de la chambre antérieure (qui n’était pas mesurée avec les premiers biomètres). Mais on conçoit que la prédiction de la position effective de l’implant sera effectuée d’autant plus loin de la cornée que l’oeil est long.
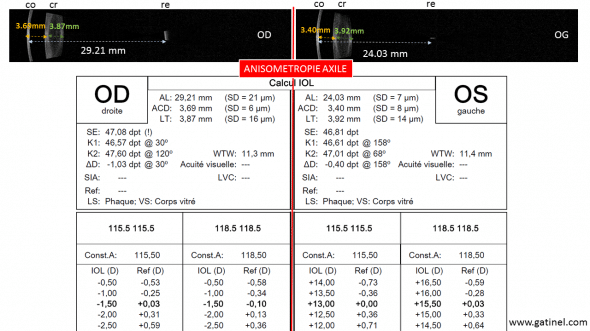
Biométrie (IOL Master 700, Zeiss) chez un patient présentant une anisométropie importante: l’oeil droit est plus myope, car il est plus long de quelques milimètres. Sa chambre antérieure est plus profonde du côté de l’oeil plus long, ce qui laisse présager une position effective finale plus grande (distance cornée / implant) du côté droit que du côté gauche. La kératométrie est relativement similaire des deux côtés. La plupat des formules de calcul d’implant de 3e génération utilisent la valeur de la longueur axiale pour la prédiction de la position effective de l’implant.
Plutôt que « calcul » de la puissance de l’implant, il serait peut être préférable d’utiliser le vocable « prédiction« , car le fait de ne pouvoir prédire l’exacte position de l’implant dans l’oeil induit une certaine incertitude quant au résultat final (cette incertitude est cependant limitée à une à deux dioptries au maximum dans la plupart des cas d’yeux sans antécédents ophtalmologiques).
Puissance optique des implants
Elle s’exprime en dioptrie (symbole D :ex: 22 D) et correspond à la vergence de l’implant (dans les milieux oculaires); pour les implants multifocaux, il s’agit de la vergence du foyer destiné à focaliser les rayons issus des sources lointaines (vision de loin). Pour les implants toriques, il s’agit généralement de la puissance « moyenne » (autour de laquelle se distribue la variation de puissance nécessaire à la correction de l’astigmatisme). Comme souligné précédemment, il n’y a pas de rapport direct entre la puissance de l’implant et la correction en lunette préopératoire. En moyenne, les yeux emmétropes bénéficient d’implants dont la puissance est proche de 22 D. Les yeux myopes, plus longs, reçoivent généralement des implants de puissance plus faible, et les yeux hypermétropes, plus courts, des implants de puissance plus élevée. La puissance des implants varie par pas de 0.5D. En moyenne, une modification de 1 dioptrie de la puissance d’un implant provoque un changement de 0.7 D dans la correction en verre de lunette (ceci est lié à la variation de la distance entre le plan du verre de lunette et celui de l’implant).
Exemple de biométrie par mesure ultrasonore
Les données biométriques peuvent être recueillies grâce à une mesure échographique bi dimensionnelle (B scan) : ce type de recueil est préféré ou complète la mesure optique (interférométrique) dans quelques indications, notamment chez les myopes forts, ou quand il existe une réduction de la transparence des milieux optiques prononcée (taie cornéenne, cataracte très évoluée, etc.). Avant l’avènement de la biométrie optique, la biométrie ultra sonore axiale (en mode A) était utilisée pour déterminer la longueur axiale de l’oeil; cette technique était beaucoup moins précise car manuelle et dépendante de l’opérateur. L’échographie en mode B permet de recueillir des données anatomiques ce qui permet de mieux estimer la longueur de l’oeil examiné.
Pour mesurer la longueur de l’oeil, on se fonde sur le temps mis par les ondes ultrasonores à traverser l’oeil; la vitesse de déplacement des ondes ultrasonores varie en fonction du milieu traversé (elle est supérieure dans le cristallin). En moyenne, elle est proche de 1550 mètres par seconde, mais elle varie (plus élevée dans le cristallin).
La figure suivante montre un exemple de la coupe échographique ainsi obtenue de l’œil mesuré. A partir du recueil de la longueur axiale, et de la mesure de la kératométrie (accomplie au moyen d’un autre instrument :topographe, kératomètre), une puissance d’implant « emmétropisante » peut être obtenue.
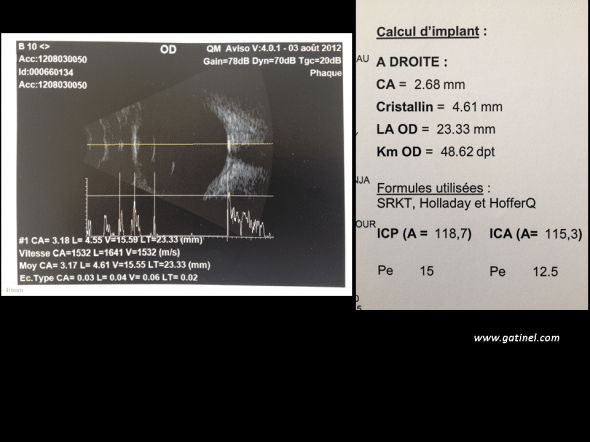
L’écho biométrie en mode B permet de mesurer la longueur de l’œil et visualiser en coupe les principaux éléments de celui-ci de part l’écho qu’il produit: successivement, on observe un pic pour la cornée, les faces antérieures et postérieures du cristallin, et la rétine. A partir de la position de ces échos dans le temps, on peut estimer la profondeur anatomique de la chambre antérieure est de 3.17 mm, l’épaisseur du cristallin de 4.61 mm, et la longueur du segment postérieur (cavité vitréenne) 15.55 mm. La longueur totale du globe oculaire (longueur axiale) est de 23.33 mm. En utilisant cette valeur et celle de la kératométrie (48.62 mm), le calcul utilisant diverse formules converge vers la valeur de 15 Dioptries pour l’emmétropie (la constante A utilisée est de 118.7).
En conclusion, l’examen biométrique oculaire est indispensable avant chirurgie de la cataracte avec pose d’un implant. Il permet de prédire la puissance de l’implant destiné à procurer à l’oeil, en plus de la restitution des la transparence des milieux, une réfraction adaptée au souhait du patient. Cette prédiction est entachée d’une certaine imprécision, que les formules de calcul les plus récentes visent à réduire au maximum.

Bonjour
Je suis optometrist et j’aurais voulu savoir si vous proposez une formation de biométrie ( calcul de lentilles toric, …)
Merci d’avance
On m’a diagnostiqué un HSV (herpès) il y a quelques années et mon médecin m’a dit qu’il n’existait pas de traitement définitif. On m’a prescrit des médicaments pour ralentir la progression du virus. Au début, ce n’était pas si grave, jusqu’à ce que la maladie atteigne un stade où j’avais des difficultés à vaquer à mes occupations quotidiennes : je ressentais constamment des douleurs au pénis et des cloques autour des parties génitales. J’étais complètement anéantie et j’avais même honte de me plaindre. J’ai lu une publication sur un médecin, le Dr Water, qui utilisait des plantes médicinales pour soigner des maladies comme l’herpès, le papillomavirus humain, la SLA, le diabète, le VIH, etc. J’ai décidé de le contacter par e-mail. Après quelques échanges, j’ai commandé son médicament. Il l’a préparé et me l’a expédié. Une fois le médicament reçu, je l’ai pris selon ses instructions. Après l’avoir utilisé comme indiqué, quelques semaines plus tard, je suis allée à l’hôpital pour une analyse de sang, qui s’est révélée négative. À ma grande surprise, j’ai été guérie de ce virus tenace grâce à un simple produit à base de plantes. C’est pourquoi je partage ici mon témoignage afin de sensibiliser le plus grand nombre possible et d’aider les autres à en bénéficier et à guérir. Pour obtenir de l’aide, contactez-le par e-mail : {DRWATERHIVCURECENTRE@ GMAILCOM} ou par WhatsApp (+2349050205019).
Je tiens à remercier le docteur O.WATER pour le médicament à base de plantes qu’il m’a donné, à moi et à ma fille. Je souffrais de VIH et d’épidémies d’herpès simplex sur tout mon appareil génital lorsque j’ai donné naissance à ma fille et c’est ainsi que ma fille a contracté la maladie indirectement de moi, mais à Dieu soit la gloire que je sois guérie grâce au médicament à base de plantes que le docteur O.WATER m’a donné. Je veux utiliser ce moyen pour dire à tout le monde que la solution à notre maladie est arrivée, je voudrais donc que vous contactiez ce grand guérisseur sur son adresse e-mail : DRWATERHIVCURECENTRE@ GMAILCOM et Whatsapp +2349050205019. Je suis vraiment heureuse aujourd’hui que ma fille et moi soyons guéries du VIH et de l’herpès, nous sommes maintenant négatifs après l’utilisation de son médicament à base de plantes, mon médecin spécialiste le confirme. Une fois de plus, je dis un grand merci au docteur O.WATER pour vos mains guérisseuses sur ma vie et celle de ma fille.
Toutes mes excuses à tous, mais je dois partager ceci pour aider une ou deux personnes. Que dire de plus à son sujet ? Aujourd’hui, je suis tout aussi reconnaissante envers le Dr Water, car je suis enfin guérie du VIH qui me rongeait depuis plus d’un an et six mois. Après avoir cherché différents moyens de guérir, sans succès, je peux aujourd’hui témoigner avec audace au monde entier qu’avec l’aide de la phytothérapie, j’ai retrouvé la santé et la force en quelques semaines seulement, après avoir contacté un excellent herboriste, grâce à un blog consacré à la guérison du VIH. Il y a quelques semaines, j’ai lu un article d’une femme expliquant comment elle avait été guérie grâce à des plantes médicinales que le Dr Water lui avait envoyées. J’ai donc décidé de tenter l’expérience de cet homme formidable en le contactant via son adresse e-mail et son numéro de portable. Je lui ai expliqué mon problème, et il m’a promis que tout irait bien une fois que j’aurais fini d’utiliser son remède. Il me fallait absolument croire en lui, et c’est ce que j’ai fait. Et voilà, je suis aujourd’hui très heureuse. C’était comme par magie lorsque mon test sanguin s’est révélé négatif. C’est pourquoi je suis venue ici pour témoigner au monde entier et partager mon expérience, car je sais que de nombreuses personnes cherchent également un remède à une maladie ou une autre. Vous pouvez également contacter le Dr Water dès maintenant pour ses plantes médicinales, via son WhatsApp au +2349050205019. Écrivez-lui dès aujourd’hui ; je suis convaincue qu’il sera capable de vous guérir vous-même du VIH/sida et de guérir toutes ces maladies : hépatite B, verrues HPV, cancer, herpès simplex, SLA, diabète de type 1 et 2, stérilité masculine et féminine.
Nous pouvons la calculer aussi partout aussitôt une géstion murale
La réduction de la correction est liée à la cataracte (myopisation d’indice, ce qui induit une réduction de la correction chez les patients initialement hypermétropes). L’astigmatisme de l’oeil droit est modéré, et je ne peut pas expliquer les larmoiements et la vision double; L’implant est une lentille intraoculaire de puissance 24.5 D (Artis). Toute intervention de cataracte comporte la pose d’un implant.
Bonjour Docteur,
J’ai 74 ans. En octobre 2022, lors d’un contrôle habituel, mon ophtalmo m’informa d’une légère cataracte qu’il jugeait inutile d’opérer pour l’instant puisqu’elle ne me gênait nullement. Je lui signalais une absence de vision de certaines lettres à la lecture, un « trou noir ». Un OCT décela un trou maculaire à l’oeil gauche, de petite dimension. Le chirurgien envisagea l’opération pour janvier 23. Il m’assura que cette opération entraînant automatiquement une cataracte dans un délai de 3 à 18 mois, il fallait mettre en place un implant. J’étais très réticente pour cet implant.
L’opération fut réalisée le 23 janvier 2023, trou maculaire et implant.
Il ne m’a été remis aucune « étiquette » mentionnant les caractéristiques de l’implant.
Lors d’une visite post-opératoire, le chirurgien déclara le trou maculaire fermé. Il s’aperçu que le fil suturant la cornée était toujours en place ; il le retira le 22 février soit un mois après l’intervention . Des lunettes avec correction définitive furent prescrites. Je les porte depuis 1 mois.
Actuellement, les problèmes sont les suivants : forte pression dans l’OG opéré, maux de tête, larmoiements constants et abondants, et surtout vision double en particulier vers le haut et le bas, ce qui occasionne vertiges et troubles de l’équilibre. Seul un champ de vision très réduit, à mi-hauteur est quasi normal.
Avant l’opération, lunettes portées, verres progressifs :
OD + 3,75 = 10/10 Add 3,00
OG + 3,25 (+0,25 à 58°) = 10/10 Add 3,00
Examen de la vue, en octobre 2022, lors de la découverte du trou maculaire :
Réfraction finale :
OD + 2,50 (+0.50 à 15°) = 9/10 Add 3,00
OG + 2,25 (+0.25 à 20°) = 5/10 Add 3,00
Lunettes actuelles, portées depuis un mois, verres progressifs.
OD : +2.75 (-0,50 100°) Add 3,00
OG : 0,00 (-0.50 170°) Add 3,00
Je constate que l’oeil droit, non opéré, a une correction plus faible qu’auparavant. Pourquoi ?
Le fait d’avoir retiré le fils de suture de la cornée seulement un mois après l’intervention a-t-il eu une incidence sur l’astigmatisme ?
Pensez-vous que les problèmes de vision double, pression dans l’oeil, maux de tête, larmoiements vont s’estomper ?Le chirurgien m’a prescrit des gouttes pour les larmoiements mais ceci n’a pas d’effet.
Je n’ai aucune référence de l’implant, la clinique ne m’ayant remis aucun document lors de ma sortie.
Le compte rendu opératoire mentionne : implant ARTIS +24,5 D SN : 2216169007.
Merci d’avance pour vos réponses.
Recevez mes salutations distinguées.
La biométrie peut être effectuée avec une pupille dilatée, sans que cela modifie véritablement les valeurs requises pour le calcul d’implant.
Est-ce que la biométrie peut être faite lors de la première rencontre avec l’ophtalmologiste et que la pupille est dilatée ou s’il faut une autre rencontre sans dilatation de la pupille. Merci.
Bonjour Docteur
J’ai été opérée de la cataracte de l’oeil droit il y a 3 semaines. J’avais demandé un implant qui corrige la presbytie.
Depuis je vois flou de l’oeil droit (exception faite si je lis à proximité d’une lumière très éclairante.)
Je n’ai pas osé me faire opérer de l’oeil gauche car un tel flou des 2 yeux ne serait pas supportable.
J’en ai bien entendu parlé au chirurgien auquel j’ai posé les 3 questions suivantes:
Peut-on retirer cet implant et le remplacer par un monofocal ?
Peut-on mettre un mono focal à l’oeil gauche?
Des lunettes avec un verre neutre à droite peuvent-elles être envisagées ?
La réponse fut un NON laconique dans les 3 cas.
Pouvez-vous me donner votre avis ?
Je vous envoie les caractéristiques de l’implant :
Carl Zeiss Meditec AG
MD AT LISA tri 839MP
D: +22.0
SN 25220821E012
T=11.0 body =6.0
UDI-DI : 04049336786925
near add : +3,33
int add : + 1,66
Je vous remercie.
Il est possible de corriger l’oeil gauche pour la vision de loin (comprendre la différence entre le résultat attendu et obtenu de l’oeil droit paraît important dans ce contexte). La différence entre les deux yeux peut tout à fait être bien supportée. Si tel n’était pas le cas, une correction par chirurgie réfractive de l’oeil droit (LASIK ou PKR) est envisageable.
Les éléments fournis ne sont pas en rapport avec les implants posés mais la cornée. Vous devriez avoir reçu des « étiquettes » comportant la marque, le modèle, et la puissance des implants posés. Y figurent les informations qui permettent de connaître le type d’implant posé.
bonjour
suite a mon opération de la cataracte il y a 1 mois
pouvez vous me confirmer avec la mesure de dioptries qu’ il s’agit bien d un implant bifocaux
puissance théorique de l implant: dioptries
Astigmatisme préopératoire
44.75 83°,4600 173°(-125) / 44.75 100°,45.25 10°(-0.50)100°
merci de votre réponse car de loin il n y a aucune amélioration
bien cordialements
Bonjour, opérée de la cataracte (œil droit), il y a 3 semaines, implant monofocal, je suis très déçue quant au résultat : ma myopie initiale de -6 d est passée à -1,5, alors que je souhaitais avoir une acuité visuelle de 10/10 de loin.
J’hésite à me faire opérer de l’œil gauche. Puis-je demander une compensation qui me permettrait, d’avoir une vision parfaite de loin de cet œil et cela générera-t-il un problème d’adaptation ? Merci
Bonjour,
A 65 ans j’ai été opéré il y a 4 semaines pour une cataracte avancée de l’œil gauche, l’œil droit ayant une cataracte légère.
Mon acuité avant opération était de:
VOD 8/10 ac et P2 ac
VOG 5/10 ac et P2 ac, ( tonus 18 ODG)
Depuis l’opération: l’œil droit et l’œil gauche pris séparément voient normalement, l’œil opéré gauche ayant une acuité de 10/10 corrigée.
PROBLÈME : Si je regarde normalement avec les deux yeux, j’ai une grosse sensation de loucher, avec ou sans lunette à ma vue. Je ne peux pas conduire un véhicule, ni une bicyclette, je ne peux pas remplir un verre d’eau, ni descendre normalement un escalier. Ma vie est devenue un enfer !!
(La seule solution actuelle pour voir normalement est de cacher un œil)
Mon œil opéré renvoi une image plus claire et plus grande que l’autre.
Physiquement, la pupille de l’œil opéré est en étoile et plus grosse d’environ une fois et demi fois la pupille droite.
Mon sentiment est que chaque œil renvoi une image différente que le cerveau ne superpose pas.
Depuis le lendemain de l’intervention à maintenant, il n’y a aucune évolution.
Le chirurgien qui m’a opéré se montre très désinvolte et refuse de donner une suite à mon pb.
Il m’a indiqué que c’était une intervention difficile, le cristallin était dur, et l’œil ne s’est pas dilaté malgré tous les produits utilisés. Sa réponse est : c’est normal la dilatation sequellaire par rapport à l’œil droit, c’est ça où on n’opérait pas la cataracte.
L’implant mis en place : HOYA Model XY1 +16.00D diamètre : T 13.0mm B 6.0mm
Correction des verres avant opération :
OD -4
OG (50-2) -6
Correction des verres après opération :
OD -4,5
OG (75-1) -1,20
Acuité après opération, sans verre correcteurs
VOD 2/10
VOG 2/10
Qu’en pensez-vous ? Y a t-il un risque que l’implant soit mal posé ?
Vais-je un jour retrouver une vue normale ?
Merci pour votre
Bien cordialement
La biométrie peut être effectuée à distance (en avance sur) l’intervention, les paramètres d’intérêt pour le calcul de l’implant ne sont pas susceptibles d’évoluer significativement (le degré de cataracte n’intervient pas directement dans cette mesure). Concernant votre première question, pourquoi effectuez vous l’intervention si vous n’êtes pas gênée et que vous trouvez que votre vision est bonne? L’indication de la chirurgie est avant tout fonctionelle (traiter des symptômes visuels liés à la cataracte: voile, éblouissements, halos, gêne à la lecture, etc.). Si vous n’êtes pas gênée visuellement il n’y a a priori pas d’urgence pour effectuer une chirurgie, même s’il existe une cataracte débutante.
Bonjour,
J’ai 60 ans et j’ai un cataracte à l’œil gauche et je dois me faire opérer. J’ai une bonne vision en général et j’utilise des verres progressifs pour la lecture seulement et travailler à l’ordinateur. J’ai une bonne vision de loin.
Quel type d’implant me conseilleriez-vous? Est-ce que je peux espacer l’examen de biométrie et l’opération ou i est souhaitable que la biométrie soit faite proche à la date d’opération.
Je vous remercie à l’avance.
Salutations cordiales.
Non cet examen de biométrie pour le calcul de l’implant est effectué sans dilatation pupillaire
Bonjour, l’examen biométrique de calcul d’implant, en amont de la chirurgie de la cataracte, nécessite-t’il une dilataion pupillaire, et en conséquence le besoin d’être accompagné si impossibilité de conduite?
D’avance merci
Le retrait de lentilles rigides au moins quelques jours (voire semaine selon l’aspect de la topographie cornéenne au retrait) est effectivement préférable pour bien mesurer la puissance optique de la cornée.
Bonjour docteur
Je dois être opérée de la cataracte premier oeil prochainement
Je n’ai eu aucune explication a l’hôpital mais apparemment ils m’ont fait passé les examens biométriques en juin
Mais ne sachant pas et portant des lentilles rigides, je ne les ai retirées que 5 mn avant …
Est ce normal ?
Depuis j’ai lu qu’il fallait les retirerai moins quatre jours avant les examens
Pouvez vous me le confirmer ?
Merci
J’ai aussi un glaucome et une très forte myooie
La lecture n’aura pas d’influence sur le résultat de la mesure biométrique. Le port de lunettes pourrait vous être utiles (pour corriger le loin) dans l’intervalle car effectivement vous ne pourrez faire grand chose sans lunettes (si ce n’est de la lecture rapprochée) d’ici là.
Bonjour Docteur,
J ai RDV chez mon ophtalmo le 29 novembre pour une biométrie en vue d une opération l an prochain pour me corriger ma myopie. J ai -13 et -11 dioptries, pas de cataracte.
Je porte des lentilles rigides et n ai pas de lunettes si ce n est des lunettes pour ma presbytie.
Mon ophtalmo m a donc demandé de retirer mes lentilles 15 jours avant le RDV pour la biométrie.
Ma question est la suivante, puisque je vais être dans le flou total durant 15 jours car pas de lunettes pour y remédier, vous comprendrez que mes activités vont être très limitées…
Puis je tout de même me permettre de lire de très près sans que cela ait une incidence sur l examen à venir ou faut il mieux que je m abstienne ?
Je vous remercie par avance.
Bien cordialement.
Les « obstacles » à l’implantation multifocale sont divers: certains patients sont désireux de conserver des lunettes (ex: de loin pour les myopes, on vise alors une correction résiduelle faible avec des implants monofocaux, qui permet au patient de lire sans lunettes à environ 40 cm). Certains patients souhaitent bénéficier de la meilleure vision possible de loin (pas de halos, contraste maximal), et n’ont rien contre porter des lunettes de lecture – et parfois l’obstacle est financier. Il existe aussi des contre indications ophtalmologiques (glaucome avancé, DMLA, myopie forte, etc.) à l’implantation multifocale. Enfin, certains chirurgiens ne proposent pas systématiquement ces implants à leurs patients, pour des raisons diverses (méconaissance des règles d’usage, désir de ne pas augmenter les attentes du patient étant donné que les implants multifocaux exigent une technique irréprochable, un calcul biométrique précis, etc.). On observe que pour certains chirurgiens, le taux d’implantation multifocale est proche de 50% ou plus. Chez d’autres, elle est de 0%. Ceci reflète bien une disposition à proposer et poser ces implants.
Bonjour
Je dois me faire opérer de la cataracte oeil gauche. j’ai 65 ans et souffre uniquement de presbystie
j’ai lu que 95 % des patients recevaient un implant monofocal.
Je m’interroge car il me semble que les implants multifocaux sont une avancée puisqu’ils permettent de se passer de lunettes.
Alors pourquoi seulement 5% qui ont accès, est-ce un problème d’ordre financier ou médical.
merci par avance.
Cordialement
Il est effectivement plus délicat d’opérer les yeux petits (courts) et dans ces situations il est recommandé de recourir à une anesthésie par injection locale (ou générale), c’est à dire éviter les anesthésies topiques pures. Il faut également que l’anesthésiste contrôle en amont la pression artérielle pour éviter les poussées. Une intervention de la cataracte n’est pas urgente dans votre cas, mais si la gêne visuelle s’accentue, il faudra envisager l’intervention à un moment donné.
Bonjour. J’ ai subi hier un examen en vue d’une opération de la cataracte dont la date était déjà fixée,. Malheureusement suite à cet examen mon ophtalmologiste m’à annoncé que l’ intervention allait être très compliquée et comporterait de grands risques en raison de la longueur de mon oeil. Il est très petit, 21 mm, et donc des risques qui’pourraient aboutir à la cécité. .. donc, en accord avec mon médecin, il a été décidé d’ attendre et de refaire le point dans 6 mois. J’ ai également subi il y a 2 mois une séance de laser de chaque oeil afin d’ élargir l’angle rétréci par la cataracte qui avait évolué et qui risquait de m’ occasionner un glaucome aigu… mon médecin se trouve très content du résultat. Je vous remercie de me donner votre avis quant au report de cette intervention. Jean suis âgée de 72 ans et ne souffre d’ aucune autre pathologie.
A priori il n’y a aucune urgence à réaliser la chirurgie du deuxième oeil, si vous tolérez l’écart de correction ou encore pouvez corriger l’oeil droit en lentille.
Bonjour Docteur
Je suis bloqué dans un pays d’Asie pour encore des mois et j’ai pris la décision de me faire traiter l’oeil gauche : cataracte et implant pour myopie. _4.75D.
Est il nécessaire de faire le 2 ème oeil rapidement par le même docteur ? -4.50D mais pas de cataracte.
Cordialement
Il est avant tout recommandé de faire un bilan destiné à comprendre l’origine de cette absence de récupération totale. Si celle-ci demeurait incomplète, il conviendrait de réviser le choix de l’implant pour le second oeil a priori.
Bonjour,
65 ans, j’ai été opéré de la catharate oeil gauche le jeudi 11 mars 2021 avec myopie de l’oeil corrigée par lentille de contact -6, mise en place d’un implant trifocal Médicontur 640MY Pwr +19,00 D, Add +3,50 D. 6 jours aprés l’opération, ma vision de trés pres (25CM) est parfaite, mais je n’ai aucune netteté en vision intermédiare et de loin, tout est trés flou, mon ophtalmo me dit qu’une période d’adaptation peut etre longue, qu’en pensez vous ? de plus on envisage l’opération de l’oeil droit par un implant trifocal Médicontur d’ici deux mois. Mais maintenant j’hésite, si le résultat oeil gauche ne s’améliore pas. qu’en pensez vous
avec mes remerciements pour vos réponces
salutation, jean michel vinel
Il existe parfois des discordances entre le résultat observé et prédit par la biométrie oculaire. Il existe une option beaucoup plus simple que le changement d’implant pour la correction de ces « surprises réfractives »: la chirurgie réfractive cornéenne, en LASIK ou PKR. Ce geste est minimalement invasif, beaucoup moins invasif que le changement d’implant. Il est peu probable qu’une modification spontanée de la réfraction survienne dans une magnitude supérieure à 0.50D environ avec le temps.
Bonjour
J’ai été opéré de la cataracte le 3 décembre de l’œil droit et le 17 décembre de l’œil gauche. Des le lendemain de l’opération la vision de loin était parfaite avec l’œil droit par contre la myopie n’est pas corrigée intégralement pour l’oeil gauche. Le chirurgien me conseille d’attendre et me revoit le 17 janvier . Nous sommes le 26 décembre et après 8 jours de l’opération il n’y a aucune amelioration.
Si les calculs biométriques ont été correctement effectués et si la lentille correspond à ces calculs est il possible que la situation s’améliore avec le temps ? Dans le cas où cette lentille n’est pas correcte peut on en placer une qui respecte mieux les calculs de biométrie? Ce qui nécessite une nouvelle intervention ! Et après combien de temps?
Il est impossible de répondre à cette question sans données précises: réfraction visée du côté gauche, et données biométriques préopératoires notamment.
J’ai été opérée de la cataracte il y a 15j mon oeil gauche est parfait, mon oeil droit est pareil qu’avant la vue de loin n’est pas du tout corrigée, la biométrie a t’elle été faite correctement ?
Dans ce type de circonstances, il est possible d’envisager une intervention au laser (PKR) pour corriger une éventuelle myopie qui a pu être induite par l’implant posé. La précision du calcul biométrique est moindre dans le cas d’un oeil opéré de kératotomie radiaire, mais comme indiqué, il est possible de réaliser une correction laser secondaire sur la cornée pour corriger un éventuel défaut optique résiduel de type myopique ou hypermétropique (ceci peut être en tous les cas plus simple que de changer un implant).
Bonjour , je me suis fait opéré le 29 sept 2020 de l œil G par implant pour récupérer une vision de loin AT TORBI 20 + 4.50 à 85 degrés mais le résultat est inverse , j y vois correctement de près et non de loin ! j ai subi il y a une trentaine d années une kératotomie radiare 4 incisions pour une petite myopie 1.5.
Il était prévu pour l autre oeil une correction de prés AT Torbi 22 à 40 degrés mais nous l avons différé en attendant une éventuelle évolution mais rien n ‘a changé en 3 semaines .
Merci pour votre expertise et votre conseil.
Effectivement, la détermination de la puissance de l’implant à poser ne dépend pas d’un test de lecture, mais de mesures anatomiques (biométrie) et statistiques (prédiction de la position de l’implant dans l’œil).
Bonjour,
Si j’ai bien compris, la puissance de l’implant est calculée à l’aide du biomètre optique et le test de lecture n’entre pas dans le calcul. Je suis un peu angoissée par rapport à ça car lors du test de lecture, j’avais les yeux très secs et je portais un masque, j’ai eu l’impression que ma vision était faussée.
Pouvez-vous me confirmer qu’il n’y a pas d’incidence ou dois-je revoir mon ophtalmo avant l’intervention ? Je vous remercie.
Il serait utile de connaître le type exact d’implant posé. Les implants qui procurent une vision de loin et intermédiaire ne sont pas réellement monofocaux (ceci est contradictoire avec cette plage de vision étendue). Il peut s’agir d’implants à profondeur de champ étendue (Eyeon) on d’implant dits EDOF de type Symfony; ces derniers sont des implants bifocaux avec une vision de loin et une vision intermédiaire (pas de vision de près). Quel que soit le type exact d’implant posé, les implants EDOF ou à profondeur étendue ne donnent pas de vision de près. Seules les implants trifocaux sont à même de procurer une vision nette aux trois foyers.
Bonjour,
Je viens d être operé à 45 ans de l.oeil gauche le 18 août 2020 et le l.oeil droit 29 septembre 2020 œil droit.
On m’a posé des implants nouvelle génération monofocale Johnson Johnson diopter +22.OD ot : 13 mme oB 6 : 6 mm pour les 2 yeux vision de loin et vision intermédiaire
J y vois mal de près et je vois des halos la nuit phare de voiture et feux rouge.
A la base je n’avais pas de problème de vue,
Juste un traitement à base de cortisone qui m.a fait dés cataracte
Vous pensez que les halos vont disparaître et la vue de près peut s amelioré,
Car les interventions sont récentes.
Je vous remercie
Ceci est affaire de « goût », mais il est généralement conseillé de laisser une myopie légère chez les forts myopes opérés de cataracte; expliquez à votre chirurgien que ceci est votre souhait (vous voulez pouvoir continuer à lire sans lunettes), et que vous avez accepté l’idée d’une légère correction de loin au décours de l’intervention (lentilles ou lunettes, etc.).
Je dois subir une opération de la cataracte à l’oeil gauche à la suite de l’ablation d’une membrane épiretinienne. J’ai 57 ans et une forte myopie aux deux yeux. L’oeil droit ne nécessite pas une opération de la cataracte et la myopie est de – 12,5. Le chirurgien me conseille de corriger complètement la myopie à gauche, une lentille pour l’oeil droit et des lunettes de lecture. Je pensais opter pour une myopie résiduelle de -3 à l’oeil gauche pour une vision de près. Que conseillez-vous ? Merci d’avance pour votre réponse.
Bien à vous
La chambre antérieure est effectivement présente (espace compris entre la cornée en avant, et le plan de l’iris en arrière), mais elle communique alors avec la chambre postérieure de l’oeil.
Bonjour Docteur,
Si je comprends bien les schémas, une fois le cristallin retiré si un implant n’est pas remit nous avons « plus » de chambre anterieure ?
Du moins nous ne pouvons plus la mesurer ?
Bien Cordialement
Le retrait des lentilles souples devrait idéalement avoir lieu 48 heures auaparavant, pour que la fiabilité de la mesure biométrique soit optimale.
bonjour
je suis contente de pouvoir me faire opere car jai une forte myopie (-18.75.oeil gauche )et (-15.75 oeil droit ) en lentille rigides je porte actuellement des lentille souple journaliere car je ne suporte plus me lentille rigides jai des lunettes que je met qua la maison parcque je suis géner de les mettre a lexterieur bref …..
mon ophtalmo me propose de remplacer le cristallin comme pour une operation cataracte mais elle ne ma pas preciser sil faudrai que je retire mes lentilles souple avant les tests preoperatoire
en sachant que la tecnologie du materiel est utilider peut faire ce calcul sans un delai tres long sans lentille avant ces test
je pourrai les retirer mardi a 17h et les tests auront lieu jeudi matin 8h30 est ce sufisant ?
jangoisse sur le fait de devoir les retirer beaucoup plutot. merci de me repondre sa maiderai beaucoup .
Le calcul biométrique de la puissance de l’implant peut effectivement être réalisé sur l’oeil non traumatisé. Cependant la présence d’un traumatisme cornéen peut avoir modifié la puissance optique de la cornée de cet oeil, et cela aura une influence sur le résultat optique. Le choix de la puissance optiamale pourra être effectué (il s’agit toutefois d’une prédiction) en considérant l’ensemble de ces éléments.
Il est difficile de répondre à votre question sans connaître le degré de correction actuel. En général, les patients s’accommodent de cette phase de transition entre les deux interventions, surtout si l’oeil opéré en premier récupère rapidement.
Bonjour,
Mon oeil gauche doit être opéré de la cataracte après avoir été opéré d’une membrane épirétinienne en décembre dernier. Compte tenu de cette intervention, mon Ophtalmo m’a dit qu’il était nécessaire de faire un implant et que je devais aussi faire subir les mêmes interventions à l’oeil droit compte tenu de la correction à l’oeil droit, mon cerveau n’accommoderait pas. Les deux interventions doivent se faire à 15 jours d’intervalle et le contrôle des interventions se fera un mois après.
Ma question, quelle sera mon acuité visuelle après les opérations alors que mes lunettes ne seront pas adaptées ?
Bonjour
Comment peut on faire un calcul d implant sur un oeil traumatisé qui presente une plaie de cornee transfixiante et une cataracte traumatique et qu on peut faire une implantation primaire ou secondaire
Est ce que faire le calcul au niveau de l oeil adelphe est faisable
Merci pr votre reponse
Ceci correspond au symptôme d’anéisoconie. En général, il est lié à une différence importante de correction entre les deux yeux. Une fois l’autre oeil opéré, cette sensation devrait disparaître – à condition que la correction visée soit sensiblement la même entre les deux yeux.
La taille des objets vus par mon œil gauche opéré de la cataracte et la taille du même objet vu par mon œil droit non encore opéré est différente.
Cela est_il dû à la position de l’implant dans l’axe de l’œil ?
Il est preferable de ne pas utiliser d’implants multifocaux dans votre cas, en raison des antecedents de chirurgie refractive type kératotomie radiaire (deformation cornéenne avec astigmatisme irrégulier, incompatible a priori avec un implant multifocal).
Bonjour
Je dois être opérée de la cataracte, les examens ont été faits, mais on m’ a dit que la transparence des milieux optiques de mes yeux est tellement réduite,m( cataracte trop avancée, forte myopie et cicatrices trop grandes sur la cornée après keratotomie mal passée, ce qui déforme légèrement la cornée) qu’ on ne peut pas calculer l’ implanté avec précision impeccable ( biométrie optique et échographie ont ete faits), et que les implants multifocaux ne peuvent pas être mis car peu calculables- je dois me contenter par les implants monofocaux.
Est- ce vraiment le cas? Puis- je recevoir des implants multifocaux même malgré la diminution prononcée de la transparence des milieux optiques de mes yeux? Et dans quel cas la pose des implants multifocaux n’ est pas vraiment recommandée?
Merci
Même si la carte n’est pas disponible, vous pouvez simplement demander à votre chirurgien qu’il vous communique de type et la puissance de l’implant posé au cours de la chirurgie de la cataracte de l’oeil gauche.
Bonjour,
J ai été de cataracte récemment.
Pour l œil droit il m a été remis une carte d identification d implant.
Par contre pour l œil gauche il n y a pas moyen de l obtenir , et deux mois après l intervention je ressens toujours une gêne (un voile) dans le coin externe de l œil.
Le chirurgien me dit que cette carte n est pas du tout utile .
Est ce normal ?
Merci d avance pour votre réponse.
La puissance des implants qui doivent être posé ne permet pas, sans accéder à d’autres informations biométriques, de prédire quelle sera la correction résiduelle éventuelle après la chirurgie. En général, les résultats de la chirurgie de la cataracte chez les patients sont excellents, car la correction simultanée de la cataracte et de la myopie forte procure une amélioration spectaculaire de la vision.
Bonjour je vais bientot me faire operer de la catarcte .Je suis fort myope -20 et -19.Il va me poser un implant de -4 et -5. Es ce un bon pronostique.
La dilatation n’est pas nécessaire ni recommandée pour effectuer une biométrie oculaire pour le calcul d’implant en chirurgie de la cataracte.
Pour effectuer une biométrie en prévision d’une opération pour cataracte, l’ophtalmo doit-il dilater le cristallin avec des gouttes comme lors d’un examen?
Ma recommandation est d’attendre qu’une amélioration survienne, grâce à un phénomène d’adaptation. Si ceci n’était pas le cas, il serait toujours possible, a priori, de réaliser une chirurgie réfractive cornéenne dans le futur pour modifier la correction d’un oeil (ou les deux) – en LASIK ou PKR par exemple.
bonjour
j’ai été opérée la semaine dernière de la cataracte
mon oeil opéré voit très bien de près ce qui était prévu (implant monofocal) et l’autre voit bien de loin.
en revanche la combinaison des deux n’est pas confortable j’ai une impression de flou et surtout d’éblouissement
la bascule avait été décidée parce qu’avant l’opération elle s’était déjà établie naturellement
mon ophtalmo et mon chirurgien me disent que si ce n’est pas parfait maintenant il est peu probable que cela évolue positivement et que si je veux me faire réopérer pour mettre un implant vision de loin il faut le faire de suite
j’ai consulté un autre ophtalmo et un opticien qui m’ont conseillé d’attendre et ont été rassurants sur l’évolution à terme
pensez vous que cela peut encore s’améliorer naturellement, avez vous eu des cas similaires? quelle serait votre recommandation?
La vision intermédiaire n’était pas assurée par les premières implants multifocaux (généralement bifocaux pour la vision de loin et de près). Cependant, il devrait être possible de corriger la vision intermédiaire (70/80 cm) avec des lunettes bien ajustées. Faites un point précis en concertation avec votre ophtalmologiste et opticien.
Bonjour,
Ma fille a aujourd’hui 18 ans. Elle a été opérée d’une cataracte congenitale bilaterale en 2004 et 2006 (necker Pr Dufier) avec pose d’implants multifocaux. Elle a cependant toujours eu besoin de porter des verres progressifs, la vision de près est longtemps restée instable. Aujourd’hui, il semble qu’elle a moins besoin de l’ajout du progressif pour la vision de près , et sa vision de loin est meilleure (myopie davantage corrigee pour obtenir meilleure acuité ) mais gros soucis : elle ne voit pas net dans sa vision intermédiaire. Plusieurs tentatives: verre eyezen avec petit ajout de confort, puis progressif +2, puis +2,75…rien n’y fait la vision intermédiaire reste floue. S’agit il selon vous d’un problème technique et d’ajustement de la correction? Ou cela peut il venir d’un dysfonctionnement de l’implant lui-même ? Je crois qu’un changement d’implant reste par ailleurs déconseillé du fait des adherences et présente des risques…merci de votre réponse.
Il est difficile de vous donner une méthode éprouvée dans ce contexte où la réfraction subjective est généralement fluctuante en raison de l’importance de l’astigmatisme irrégulier, qui affecte effectivement et conjointement cornée antérieure et postérieure. Dans ce genre de situation, on peut considérer que l’astigmatisme postérieur est cette fois ci « parallèle » géométriquement (toricité identique, mais astigmatisme induit de signe opposé d’un point de vue optique en raison du gradient d’indice inverse). Il est alors préférable d’être légèrement sous correcteur (alors que le nomogramme de Baylor recommande d’être plutôt surcorrecteur pour les astigmatismes inverses antérieurs).
Bonjour M. Gatinel,
Je suis opticien et travaille dans une clinique de chirurgie refractive, notamment responsable des calculs d’implants pour opération de la cataracte.
Nous utilisons habituellement entre autre les formules de Barrett, et avons constaté ses limites dans le cas de keratocône (notament en phase »2 kissing birds ») ou plus généralement dans les cas ou l’astigmatisme postérieur est plus cambré a l’horizontal.
En effet, barrett considère les ajustements basés sur l’algorythme de Baylor and Koch’reporting, ajustant le steep K en fonction de la valeur de l’astigmatisme postérieur, admettant que celui ci est plus cambré verticalement.
Quel ajustement préconisez vous dans ces cas la?
Merci pour votre retour
Salutations
A priori les implants multifocaux ne se conçoivent que pour une chirurgie réglée, sans risque de déplacement de l’implant (que laisse redouter l’ectopie), donc a priori une implantation monofocale parait plus indiquée.
Bonjour Docteur,
J’ai une ectopie cristallinienne à l’oeil gauche doublé d’une catarcte capsulaire postérieure.
Mon ophtalmo m’a prescrit un calcul d’implant.
Ma question est la suivante: Est il possible d’avoir un implant multifocal ( type technis symphony) das ce genre de situation?
Merci d’avance
Le chirurgien doit indiquer le degré de myopie visé en post opératoire. Par exemple, -2.50 D (pour la lecture), ou -1.50 D (pour une vision intermédiaire). En général, les biométries effectuées pour laisser une faible myopie résiduelle couvrent ces réfractions et pour chacune d’entre elle est indiquée la puissance théorique de l’implant à poser pour les atteindre.
J’ai vu un chirurgien ophtalmologiste pour une intervention de cataracte et qui propose de corriger en même temps ma myopie par implant .
Quels sont les renseignements nécessaires que doit donner le chirurgien pour le calcul de l’implant (biométrie) ?
Merci
La réponse à ce genre de dilemme biométrique est difficile. Au delà du problème lié à la kératométrie, il est important d’utiliser une formule qui n’utilise pas la kératométrie pour prédire à la position effective de l’implant (ex: formule de Haigis, éviter la formule SRK-T). Concernant le choix de la kératométrie, j’utilise généralement la valeur moyenne dans les 1.5 mm centraux, que fournit par exemple le topographe Pentacam. Le choix d’un implant torique est indiqué si l’astigmatisme (sa composante régulière) est important et que le patient n’a pas de correction en lentille rigide (ou n’envisage pas celle-ci), sous peine ensuite de « démasquer » l’astigmatisme de l’implant torique (en raison de la neutralisation totale ou partielle de l’astigmatisme cornéen antérieur par la lentille rigide). Pour le choix de l’axe, j’utilise la carte « Fourier transform » également fournie par le Pentacam, où on peut visualiser l’axe du cylindre dans la région centrale de la cornée. Une autre option, avec l’OPD scan, est de sélectionner le « Toric IOL display » et choisir l’axe suggéré. Dans tous les cas, l’importance de la déformation cornéenne laisse augurer d’une incertitude réfractive et d’une correction incomplète de l’astigmatisme, dont il faut prévenir le patient. Enfin, dans mon expérience, les implants toriques ont un peu plus tendance à subir des rotations postopératoires, et j’insère parfois un anneau de sac capsulaire après pose et alignement de l’implant torique pour stabiliser celui-ci.
Bonjour
J’ai un patient avec une forte myopie et un important kératocone que je dois opérer de la cataracte. J’ai du mal à déterminer la puissance de la LIO. Cela varie entre -13 et -4.50.
Il a une LA de 29.05 / ACD épith : 4.03 / K1 54.64 (75) / K2 57.81 (163) (lenstar), la kératométrie et l’axe est légèrement différente au pentacam.
Quelles formules me conseillez vous pour le calcul de son implant ? Quelles kératométries ?
Compte tenu des imprécisions de calcul, est il déconseillé de réduire son astigmatisme avec un toric ? Si non quel axe (celui du topographe, du lenstar ou de l’ARK nidek : tous 3 différents) ?
Je me suis presque dit de ne pas l’implanter et de refaire une biométrie post-opératoire, mais cela changera peut être pas grand chose après la chirurgie ….
Merci pour vos conseils
Je n’ai pas une grande expérience en ce qui concerne l’influence de la correction optique après cataracte congénitale. Un excès de pression intraoculaire peut effectivement expliquer une augmentation de la longueur axiale, mais il est plus probable qu’il s’agisse ici des conséquences de mécanismes complexes de régulation gouvernant la croissance du globe oculaire. L’équipe spécialisée qui suit votre enfant est certainement à même de vous renseigner sur ce point.
Bonjour,
Mon enfant a été opéré à 2 mois d’une cataracte unilatérale. Son oeil opéré était légèrement microphtalme avant que le cristallin ne soit enlevé (15,4 mm vs 16,5 mm) . Depuis il porte une lentille de contact à très forte correction (D: +20). Il a maintenant 15 mois et son oeil opéré est désormais plus grand que l’autre (22,1 mm vs 20,9 mm).
Cette accroissement fort de la longueur axiale peut il être une myopisation inhérente au port de la lentille de contact ? (adaptation de l’oeil à une vue de très près) ou faut-il chercher une autre raison par ailleurs (glaucome…). Merci d’avance pour votre retour. Bien cordialement.
Pour la plupart des yeux ayant achevé leur croissance, la biométrie ne se modifie pas en quelques mois. Dans le contexte d’une forte myopie (élongation du globe oculaire marquée et possiblement évolutive), il peut être intéressant de faire une biométrie de contrôle. A priori il ne devrait pas y avoir beaucoup de modifications si votre correction n’a pas beaucoup changé.
Bonjour Docteur, j’aimerai savoir si une écho biométrie faite il y a un an est encore valable pour une opération de la cataracte le mois prochain, ou vaut-il mieux la refaire pour plus de précision (myopie -10). Merci d’avance pour votre réponse. Cordialement.
Un implant de chambre antérieure est situé dans un plan qui est plus proche de celui de la cornée qu’un implant de chambre postérieure. Pour une même réfraction visée (par exemple l’emmétropie, absence de correction en vision de loin), un implant de chambre antérieure aura une puissance réduite vis à vis de celle d’un implant de chambre postérieure. Par défaut, la chirurgie de la cataracte s’effectue aujourd’hui avec une implantation de chambre postérieure, sauf situation particulière (absence de support capsulaire postérieure pour recevoir l’implant). Les biomètres disposent d’une option permettant de calculer la puissance d’un implant de chambre antérieure (en revoyant sa position et en tenant compte de certaines spécifications le cas échéant).
Bonsoir
Merci pour cet article , je voudrais si possible une précision sur le calcul d’implant pour les implants de chambre antérieur et es qu’il est possible de convertir un calcul d’implant de chambre postérieur directement pour avoir celui de l’implant de chambre antérieur. Merci de votre réponse
Merci pour ces precisions interessantes. Effectivement le 2eme oeil opéré (avec un implant de 22,5D) semble moins souffrir, tout comme le droit aussi d’ailleurs.
Toutefois dans la période de stabilisation suite a l’opération, la patiente peut voir meme un peu de pres/a mi distance, mais les douleurs reviennent vite et elle attend des lunettes pour voir de pres et a mi distance…On espere que l’oeil gauche qui devait avoir le dessus par rapport a l’oeil droit amblyope, pourra le reprendre.En attendant elle semble souffrir d’eblouissement et porte des lunettes teintées (des lunettes de soleil ordinaire)… Y aurait il une modalité de lunettes plus adéquates dans ces nouvelles conditions? Sachant que l on vient de découvrir un nouveau parametre, une parésie de la verticalité!…Cela semble exclure dejà les verres progressifs…Peut etre existe t il des verres a grande profondeur de champ, plus indiqués?
Un implant de puissance supérieure à 30D correspond à ce qui est généralement posé dans les yeux fortement hypermétropes (faible longueur axiale). A priori, l’autre oeil présente également une hypermétropie qui, si elle est corrigée en lunettes, provoque effectivement une différence de taille de l’image projetée sur la rétine entre les deux yeux : on parle d’anéisoconie (différence gênante entre les dimensions perçues d’un même objet par l’oeil droit et l’oeil gauche). L’oeil corrigé (tout ou partie) de son hypemrétropie grâce à la chirurgie de la cataracte et la pose d’un implant de forte puissance reçoit une image plus petite(ou moins grande), que l’autre oeil, non opéré et encore fortement hypermétrope, et qui a besoin d’un « verre convexe » grossissant l’image sur la rétine. Il est donc intéressant d’opérer l’oeil gauche. Le calcul de la puissance de l’implant à poser de ce côté est spécifique. Il peut tenir compte de la correction résiduelle en lunette éventuellement nécessaire à parfaire l’acuité visuelle à droite. Une fois les deux yeux opérés de cataracte et proches de l’emmétropie (grâce au remplacement du cristallin par un implant plus puissant), il n’y aura plus de différence notable entre les images perçues par les yeux (disparition de l’anéisoconie)
Bonjour,
Voila une publication vraiment interessante qui éclaire sur ces calculs prealables.
Ma tante agée qui presente une ancienne amblyopie droite s’est faite opérer de la cataracte
sur cet oeil avec la pose d’un implant de 30,5D, l’autre oeil qui ne présente qu’un debut de cataracte a été laissé en attente pendant plus d’un an et l’ophalmologiste pense la renvoyer chez le chirurgien car il estime qu’il y a une trop grande différence de taille d’image entre les deux cotés et qu’elle est responsable des douleurs et de la diplopie qui sont apparues un temps apres cette intervention, les lunettes avec prisme n’etant plus supportées. Elle m’en parle et je me demande comment va t on calculer la puissance de l’implant de l’oeil a opérer et surtout les précautions a prendre pour restaurer une vision assez confortable comme c’etait le cas avant.
En effet il semble que les calculs soient faits pour un oeil a la fois, mais ce sont les deux ensemble qui fonctionnent et il faut pouvoir superposer des images compatibles de meme taille je suppose, tout ca dans un cerveau plus tout jeune!…Merci de m’eclairer un peu sur ce point!
La pose d’un implant secondaire permettra de corriger l’hypermétropie induite par la perte du cristallin (aphakie)
Bonsoir il y a environ 1 an et des poussières j’ai pris une bille de pistolet a air ,je n’ai plus de cristallin ni de support intérieur,
le centre d’ophtalmologie de Dijon me propose un implant que doit je faire : merci de votre réponse ,salutations M Rousselot