Kératocône
Kératocône: définition, causes et facteurs de risque
Introduction:
LE KERATOCONE EST UNE PATHOLOGIE CORNENNE D’ORIGINE MECANIQUE: FROTTEMENTS OCULAIRES EXCESSIFS EN INTENSITE, FREQUENCE ET DUREE, SOUVENT ASSOCIES A UNE POSITION DE SOMMEIL IMPLIQUANT UN CONTACT PROLONGE ENTRE L’OEIL LE PLUS ATTEINT ET LA LITERIE, L’AVANT BRAS OU LA MAIN ( POSITION VENTRALE OU SUR LE COTE).
Cette vidéo permet en 10 secondes de visualiser ce qu’il se passe quand on se frotte l’oeil. Elle devrait être montrée à tous les patients qui sont susceptibles de trop se frotter les yeux, en particulier les enfants et adolescents allergiques- ou leurs parents et adultes concernés.
voir: le kératocône en bref
Lire un dossier spécial consacré au kératocône
Il est urgent de redéfinir le kératocône:
Mon expérience poussée et divers travaux entrepris par mon équipe permettent de dissiper le mystère qui entoure encore cette affection, contrairement à ce qu’enseignent encore nombre de spécialistes et traités d’ophtalmologie ou de médecine. Si vous êtes concerné ou l’un de vos proches par cette affection, lisez ce qui suit. Si on vous a proposé d’emblée une procédure chirurgicale destinée à stabiliser le kératocône (cross linking), sachez que celle-ci est en réalité SANS INTERET (pour vous) à condition que vous (ou le sujet concerné) cesse définitivement de frotter ses yeux et modifie éventuellement sa position de sommeil. Le vrai traitement du kératocône doit cibler sa cause, qui est indubitablement mécanique.
L’auteur de ce site a suivi des centaines de patients atteints de kératocône, et a compris depuis plus de 10 ans que cette affection ne relevait pas d’un processus primitivement génétique ou biomoléculaire mais traumatique. Il existe des affections d’origine génétiques à l’origine d’une fragilisation des tissus oculaires; mais le tableau ophtalmologique qu’elles induisent est bien différent.
La définition classique mais partiellement erronée du kératocône détourne du véritable enjeu à même de stabiliser et de prévenir l’évolution de la maladie; l’éviction des frottements oculaires excessifs. Les frottements oculaires excessifs sont l’ingrédient INDISPENSABLE à l’apparition d’un kératocône; leur suppression permet de prévenir (ou d’enrayer l’évolution) de l’affection.
La doxa en vigueur, malheureusement encore enseignée dans les amphithéâtre et lors des stages hosptialiers (sauf dans mon service) est celle d’une affection inéluctablement progressive d’origine inconnue est certes utile pour prescrire des traitements plus ou moins aggressifs et coûteux, en plus d’être le plus souvent inutiles ou peu efficaces: cross linking, pose d’anneaux, laser cornéen (PKR) – généralement proposés dans cette ordre. Elle est pourtant incapable d’expliquer l’incroyable hétérogénéité de la présentation du kératocône, en matière de différence entre les deux yeux, d’âge de découverte, d’atteinte sporadique au sein d’une même fratrie, de discordance entre jumeaux monozygotes… Toutes ces caractéristiques s’expliquent pourtant de manière limpide par l’historique des frottements oculaires, et des causes de ceux-ci (allergie; frottements plutôt bilatéraux, position de sommeil sur le ventre avec appui nocturne prolongé sur un oeil: atteinte plutôt unilatérale ou asymétrique, etc.). Plus les frottements oculaires apparaissent tôt dans l’existence sont effectués avec les phalanges (partie dures des doigts), plus les symptômes visuels conduisant à la découverte du kératocône sont précoces.
L’arrêt strict des frottements suffit pour enrayer l’évolution du kératocône; leur poursuite expose en revanche logiquement à une augmentation de la déformation cornéenne.
En résumé:
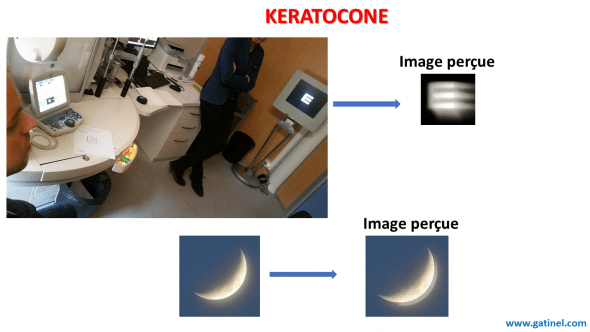
Le kératocône est une maladie oculaire dont les symptômes découlent d’une déformation de la cornée. Cette déformation de la cornée est responsable d’un astigmatisme, d’une apparition (augmentation) de la myopie, et de divers symptômes visuels dont certains ne sont pas corrigés par le port de lunettes: dédoublements d’images brillantes sur fond sombre (comme le contour qui apparait dédoublé ou triplé de la lune dans le ciel), flou visuel persistant, etc.
La cause primitive du kératocône est mécanique: tous les patients qui développent un kératocône se sont frotté les yeux de manière excessive en durée, intensité et fréquence: ces patients sont souvent allergiques, et présentent plus généralement des facteurs de risque pour les frottements oculaires chroniques: atopie, sécheresse oculaire, travail de nuit, travail prolongé sur écran, position de sommeil sur le ventre ou le côté avec appui nocturne prolongé sur un oeil ou les deux etc.
Les lésions biomécaniques irréversibles provoquées par les frottements apparaissent d’autant plus vite que la cornée est initialement plus fine, et moins résistante.
Le diagnostic du kératocône est confirmé par la réalisation d’un examen de topographie cornéenne (étude de la forme et des variations de courbure et d’épaisseur de la cornée).
L’histoire clinique du kératocône est relativement stéréotypée:
Des troubles visuels comme un flou, une sensation de dédoublement, reliés à l’apparition d’un astigmatisme myopique unilatéral ou bilatéral (généralement plus marqué d’un côté) succèdent à une période de frottements oculaires excessifs (allergie, atopie, fatigue chronique, etc.). Une topographie cornéenne est alors effectuée et révèle les anomalies suivantes sur un oeil au moins (le plus frotté): astigmatisme irrégulier, amincissement central, asymétrie.
Le délai moyen entre le début des frottements et l’apparition des premiers symptômes visuels est généralement de l’ordre de quelques années. La déformation est alors suffisamment prononcée pour engendrer les symptômes visuels. Il existe néanmoins une phase silencieuse intermédiaire, au cours de laquelle une déformation cornéenne se constitue mais est trop faible pour être à l’origine d’une dégradation visuelle perçue subjectivement par le patient.
On constate toutefois rétrospectivement l’évolution d’un astigmatisme d’origine cornéenne, souvent de direction oblique ou inverse, en rapport avec les premiers stades de déformation de la cornée sous l’effet des contraintes mécaniques répétées.
TOUT ASTIGMATISME EVOLUTIF CHEZ L’ENFANT, L’ADOLESCENT OU L’ADULTE JEUNE DOIT FAIRE SUSPECTER UN DEBUT DE DEFORMATION CORNENNE, RECHERCHER UNE HISTOIRE DE FROTTEMENTS OCULAIRES ET MOTIVER LA REALISATION D’UNE TOPOGRAPHIE CORNEENNE.
Cette déformation est parfois mise en évidence lors de la réalisation systématique d’une topographie cornéenne chez un patient qui consulte pour une chirurgie réfractive de la myopie. Ces aspects topographiques atypiques et peu prononcés font alors poser le diagnostic de « forme suspecte de kératocône », ou encore de « kératocône fruste »; au delà de débats sémantiques et étiologiques (la théorie classique est en effet impuissante à expliquer la présence de ces formes intermédiaires peu évolutives) il est crucial de bien expiquer au patient qu’il est nécessaire de ne plus se frotter les yeux aussi énergiquement (attention au démaquillage trop appuyé !).
Contrairement à ce qu’enseignent traités classiques et clament nombre de spécialistes:
Le kératocône est une affection primitivement mécanique, non primitivement génétique: la déformation cornéenne est induite par des frottements oculaires excessifs. Au départ, la déformation infligée par les frottements est de caractère élastique (réversible à l’arrêt des frottements). Au delà d’un certain seuil (qui dépend de l’intensité des frottements et des caractéristiques natives de la cornée) la déformation devient « plastique« , c’est à dire permanente.
En effet, les frottements agissent à la fois sur le plan mécanique (désorganisation de la trame des fibres collagènes de la cornée) et biomoléculaire (cytotoxicité mécanique, réaction cellulaire avec sécrétion de cytokines et enzymes pro inflammatoires). Ces mécanismes se conjuguent pour provoquer un amincissement progressif et une réduction de la rigidité cornéenne, qui sont à l’origine de la déformation plastique de la cornée.
Cette déformation explique l’apparition ou l’évolution de l’astigmatisme, qui est généralement de type myopique.
Signes visuels évocateurs:
La perception avec un œil d’un dédoublement, ou d’images multiples, fantômes, autour des sources lumineuses, peut faire rechercher la présence d’un kératocône: ces symptômes traduisent la présence d’un astigmatisme dit irrégulier. Les dédoublements et images fantômes peuvent s’atténuer avec une correction lunettes mais ils ne disparaissent pas complètement (contrairement aux symptômes provoqués par un simple astigmatisme régulier, corrigible en lunettes).
Attention, ces symptômes ne sont pas spécifiques du kératocône. Une cataracte débutante peut également provoquer un léger dédoublement des images perçues.
Quand elle est d’origine cornéenne, toute sensation de dédoublement ou d’images multiples n’est pas forcément le signe d’un kératocône, mais traduit un certain degré de réduction de la qualité optique de la cornée. Une kératite superficielle peut par exemple occasionner le même type de symptômes.
Plus le kératocône est évolué, et plus l’intensité de ces anomalies visuelle est prononcée. Dans la majorité des cas de kératocône, les images « bavent » principalement vers le bas ou en oblique vers le bas. Plus sur la vision d’un oeil atteint de kératocône ici (en anglais)
Considérations classiques à propos du kératocône
Le Kératocône, du grec kératos pour cornée et conus pour forme de cône, est défini classiquement comme une dystrophie cornéenne classiquement idiopathique (cause inconnue) bilatérale, asymétrique, non inflammatoire. Le kératocône est caractérisé par un amincissement et une déformation progressive de la cornée. Sur le plan optique, cette déformation induit de l’astigmatisme régulier et irrégulier (aberrations optiques de haut degré) provoqué par une altération marquée de la géométrie de la cornée.
On explique volontiers dans les traités que la cause du kératocône est inconnue mais qu’il existe certains facteurs de risque pour cette affection mystérieuse comme l’allergie, l’atopie, et… les frottements oculaires…
Reléguer les frottements oculaires à un rôle subalterne (celui de « facteur de risque ») est une erreur lourde de conséquences en matière de santé publique. Ceci revient à confondre corrélation et causalité, comme si l’on considérait les rayons U.V comme un facteur de risque de coup de soleil alors qu’ils en sont la cause même. Ou encore qu’un brossage trop vigoureux des dents était un facteur de risque de gingivopathie (lésion des gencives), alors que c’est bien le brossage qui provoque directement l’atteinte gingivale.

Kératocône extrêmement évolué de l’oeil gauche, consécutif à des décennies de frottements oculaires appuyés avec les phalanges des doigts. Cette image illustre le pourquoi du choix du « cône » pour rendre compte de la forme prise par le dôme cornéen dans les formes très avancées. Il est beaucoup plus difficile sinon impossible d’identifier les formes débutantes et moyennement prononcées à l’oeil nu. Le recours à la topographie cornéenne est indispensable.
Une redéfinition alternative et moderne du kératocône s’impose: elle se heurte malheureusement au conservatisme, au dogmatisme, voire à une certaine forme de paresse intellectuelle.
Redéfinir le kératocône
A la définition classique, descriptive et fonctionnelle du kératocône, l’auteur substitue une définition plus causale. Le kératocône se caractérise par l’apparition d’une déformation de la cornée responsable de symptômes visuels et de signes topographiques évocateurs.
Cette déformation est directement liée à l’action de frottements oculaires répétés, responsables d’un stress mécaniques de la cornée.
Le kératocône n’est pas une dystrophie primitive, ni une maladie génétique, mais une affection d’origine mécanique: sans frottements, sans stress mécanique répété, il n’y a pas de survenue de déformation du dôme cornéen, et donc de kératocône (voir page consacrée au rôle des frottements oculaires répétés vis à vis de l’incidence du kératocône, voir article « Eye rubbing; a sine qua non for keratoconus?« , voir article« No rub No cone, the Keraotconus Conjecture ».
Un site est totalement dédié à la compréhension de l’origine, ainsi que la prise en charge moderne du kératocône: https://defeatkeratoconus.com/.
De nombreux cas de kératocône sont présentés et illustrent le fait que les frottements oculaires sont un élément indispensable et nécessaire à la génèse du kératocône.
La vidéo suivante a été réalisée pour expliciter l’action directe des frottements sur le globe oculaire: le visionnage de ces images devrait suffire à faire passer l’envie de se frotter les yeux!
En particulier, l’étude des formes strictement unilatérales de l’affection, qui existent bel et bien, permet simplement de déduire l’élément essentiel qui est nécessaire au déclenchement du kératocône. Les patients qui se frottent un œil et épargnent l’autre (ou bien le frottent peu) présentent un kératocône unilatéral.
Ces observations sont riches en enseignement. En voici un exemple:

Dans cet exemple, le patient s’est frotté avec les phalanges – geste typique et particulièrement délétère – pendant des années, quasi exclusivement son oeil droit (il dort avec la tête en appui du même côté, ce qui explique peut être les sensations d’irritation chronique ayant conduit le patient à se frotter cet oeil vigoureusement, dès le réveil…). L’énergie mécanique véhiculée par les phalanges provoque une désorganisation architectonique du tissue cornéen et une inflammation locale qui sont responsables au bout d’un certain temps d’un amincissement et d’une déformation irrégulière mais isométrique (sans distension) de la cornée. Celle-ci ce cambre dans la région paracentrale inférieure et s’aplatit au niveau périphérique; ces modifications peuvent ici s’apprécier de manière macroscopique à l’inspection d’une macro photo en profil de la cornée de l’oeil droit. Cette cambrure augmente l’effet réfringent de la cornée. L’irrégularité est responsable de l’apparition d’un astigmatisme important. L’oeil gauche est indemne de kératocône mais présente une cornée fine: cette caractéristique ( de nature congénitale) est à même de rendre la cornée plus vulnérable à l’action de frottements excessifs.
Toutefois, la majorité des patients a tendance à se frotter les deux yeux, mais souvent de manière asymétrique: invariablement, l’œil le plus frotté est le plus atteint (la cornée est plus fine et déformée).
L’œil le plus frotté est souvent celui qui subit le plus de compression la nuit en cas de position de sommeil sur le ventre ou le côté.
L’arrêt des frottements garantit l’absence de progression de la déformation de la cornée, ce qui confirme la responsabilité directe et le caractère indispensable des frottements dans l’induction du kératocône.
En conclusion:
Le kératocône n’est pas une dystrophie idiopathique mais un syndrome d’origine acquise et mécanique, dont l’expression topographique traduit la déformation plastique de la cornée, provoquée par le stress mécanique représenté par les frottements oculaires répétés.
Cette explication est forgée sur le recueil attentif de l’histoire clinique de nombreuses observations, et un raisonnement inductif. Elle est compatible avec l’ensemble des données publiées dans la littérature médicale.
Il est crucial d’expliquer aux patients atteints et à risques (allergiques, travailleurs de nuit, sur écran, etc.) de ne pas/plus se frotter les yeux. Cette simple prescription a le potentiel d’éradiquer cette maladie, et d’en stopper la progression pour ceux qui en sont déjà atteints.
Considérer le kératocône comme une pathologie dont l’origine principale est mécanique est un bouleversement paradigmatique dans le monde ophtalmologique qui n’est pas encore pleinement admis, loin de là. Outre les aspects liés à la perte de certaines indications comme le cross-linking, le poids de l’enseignement ou certains raisonnements spécieux freinent l’adoption d’une théorie qui pourrait pourtant sauver de la progression et de l’apparition du kératocône bien des yeux. Certains praticiens soutiennent par exemple que les frottements pourraient être la conséquence du kératocône! Cette position est difficile à défendre puisqu’un simple interrogatoire des patients atteints de kératocône révèle invariablement que les frottements PRECEDENT TOUJOURS, et de plusieurs mois ou années, l’apparition des premiers symptômes du kératocône.
Ainsi, l’explication mécanique du kératocône n’est pas populaire auprès de certains praticiens qui préconisent la réalisation de certains actes chirurgicaux, souvent dès la première consultation, car elle remet justement en cause le bien fondé de leur attitude interventionniste.
Il n’est jamais urgent de réaliser un cross linking, la pose d’anneaux ou la réalisation d’une photoablation laser.

Bonjour Monsieur,
Une fois le kératocône stabiliser (suite à l’arrêt des frottements) est il possible de réaliser un PKR pour améliorer la visión ?
Quelle serait les requis en terme de stade de kératocône afin de réaliser cette chirurgie ? J’imagine que moins le kératocône est avancé et mieux sera le résultat.
Quel résultat pourrais je espérer en terme de correction de la visión ?
Cordialement.
Cordialement,
Alvarez
Bonjour docteur.
D’abord je tiens à vous remercier vivement pour toutes ces informations et éclairage sur cette maladie!!!
Je suis tombée sur votre site en recherchant des informations concernant le kératocône. J’ai lu tout votre article et c’est vraiment intéressant. J’ai fait un diagnostic de ma fille âgée de 6.5 ans apres une legere vision flou de loin
Le médecin nous a choqué de dire que le problème est lié à la kératocône
Sphère Cylindre Angle
OD : +1.25 -2.25 175°
OG : +1.75 -2.00 170°
Est ce que c’est fatal pour une fille de 6.5 ans, et quel sont les méthode les plus adaptées pour ce genre de problème
et est ce que l’arrêt de frottement des yeux peut stopper cette maladie,
Merci d’avance
En aucune manière, tant que vous vous abstenez de vous frotter les yeux. Le kératocône est une affection dont l’origine est mécanique (les frottements oculaires) et la pression intraoculaire seule ne peut expliquer la déformation observée (les cornées biomécaniquement altérées mais non frottées ne se déforment pas du tout comme dans le kératocône: elles ont tendance à « s’applatir », devenir moins cambrées).
Bonjour Docteur Gatinel,
Est-ce que la musculation avec des charges plus ou moins lourdes peuvent avoir un impacte sur l’évolution du kératocône ? Actuellement mon kc est stable (j’ai 20 ans) mais j’apprehende d’envisager la musculation.
Merci d’avance,
Non, le kératocône est provoqué par des frottements oculaires répétés et excessifs, qui au fil du temps, sont responsables d’un amincissement et d’une déformation cornéene permanente. Des coups brefs mêmes répétés peuvent en revanche propoquer d’autres types de lésions (cataracte, décollement de rétine,…)
Bonjour docteur, est ce que les coups violante sur l’oeil peuvent provoquer la keratocone? (Plusieurs coups violent s sur le mm oeil)
Un frottement isolé n’aura pas de conséquences graves, ne vous inquiétez pas. Il est toutefois observé que les patients très bien informés comme vous l’êtes sur le rôle causal des frottements peuvent être amenés à se frotter les yeux de manière inconsciente pendant la nuit. Il faut être vigilant et parfois, le port de coques oculaires de protection peut être indiqué pendant le sommeil.
Bonjour Docteur,
Je suis limite limite au niveau du keratocone et cela fait des années que je fais attention à ne plus me gratter les yeux ni à m’appuyer les yeux sur l’oreiller. Et ca marche bien. Tres bien même. Ce qui montre que c’est uniquement le grattage des yeux qui provoque cette maladie (sur a 100% apres je ne suis pas médecin).
Malheureusement, il y a deux jours, j’ai eu le malheur de me gratter les yeux avec un doigt. Je m’en veux encore. C’était en pleine nuit.
J’ai eu la vision qui etait un peu altéré (un tres tres leger flou), les yeux rouges, vous pensez que ma vue peut redevenir comme avant ce grattage ?
En vous remerciant d’avance.
Bonjour Docteur,
C’est en réponse à votre dernière réponse, j’ai 28 ans, je n’ai pas de cataracte, en tous cas tous les médecins que j’ai consulté ils ne m’ont pas parlé de cataracte, ils m’ont dit que ces aberrations sont dues à la distorsion cornéenne, je comprends mais ce que je ne comprends pas, c’est le keratocone n’évolue en aucun cas mais les aberrations oui. Ce que moi je trouve très bizarre.
Une consultation est indiquée, pour éliminer une réaction de type haze au CXL si celui ci a été réalisé récemment, ou la présence d’une cataracte, qui peut également donner ce type de symptomes
Bonjour docteur,
Je suis atteint d’un keratocone stade 3 œil gauche et stade 1 œil droit. Je voyais très bien avec sans problèmes, mais depuis quelques mois, il est devenu impossible pour moi de conduire la nuit, des aberrations très fortes, les lumières sortent de partout, quand je fais les topographies il n’y a aucune évolution donc pourquoi la vue se dégrade comme ça ? J’ai déjà fait le CXL sur l’œil gauche mais j’ai refusé pour l’œil droit car c’est l’œil qui me permet de voir très bien. Pourriez-vous me dire que cela pourrait être ? Franchement je ne sors plus la nuit car les sources lumineuses, la lumière de rue, la lumière des voitures paraissent comme des météorites et s’affichent comme de très grandes étoiles dans le champ visuel..
PS : Je ne me frotte jamais les yeux et je ne dors pas sur mon ventre pour éviter la pression sur mes yeux la nuit.
Cela dépend de l’intensité du choc reçu. Un examen ophtalmologique a du être réalisé et s’il est normal, ceci est rassurant. Néanmoins, un choc violent même unique peut provoquer à distance l’apparition d’une cataracte, ou d’un décollement de rétine. Ceci est rare, mais il est certainement indiqué de réaliser un examen du fond d’oeil régulier dans les années à venir.
Bonjour,
J’ai commencé la boxe française mais ai arrêté dès que j’ai pris un coup à l’œil. Est ce qu’un seul coup peut avoir un impact sur ma vision ?
Merci beaucoup pour votre site par ailleurs
A priori ces variations peuvent êre liées à des fluctuations de mesures, leur amplitude est relativement faible et elles ne sont pas systématisées.
Bonjour Docteur,
Je m’interroge sur la variation de données sur plusieurs topographies que j’ai réalisé.
07/11/23: Sim Ks / astig -1.6D Max 43.5D Min 41.9D thinnest point 555um axial power kerato map 45.4 MAX
23/06/22 Sim Ks / astig -1.2D Max 43.2D Min 42.0D thinnest point 554um axial power kerato map 44.8MAX
09/12/21 Sim Ks / astig -1.6D Max 43.3D Min 41.7D thinnest point 553um axial power kerato map 44.8MAX
28/05/20 Sim Ks / astig -1.4D Max 43.3D Min 41.9D thinnest point 567um axial power kerato map 45.2 MAX
AV Stable, correction en lunette identiques.
D’après mon Docteur il n’a pas d’évolution. Cependant je remarque que les valeurs fluctuent notamment la dernière. Le seul paramètre ayant changé étant le diamètre de la pupille (+ important sur la dernière topo).
Mon Docteur a bien insisté, comme vous, sur le fait de ne pas se frotter les yeux !! Je porte aussi des coquilles la nuit.
Pensez vous, d’après ces valeurs que ma déformation soit plus prononcée ou bien cela peut varier avec le diamètre de la pupille et lors de la prise des mesures ?
Je vous remercie.
Il est probable que vous dormiez « sur » un oeil ou les deux (position de sommeil ventrale, appui sur la main, l’avant bras, etc.). Ceci peut entrainer une gêne visuelle matinale, et est très souvent observé chez les patients atteints de kératocône (la position de sommeil ventrale ou sur le côté est plus fréquemment observée). Vous pouvez essayer de porter de coques oculaires de protection la nuit, afin de vérifier l’absence (ou la présence) de ces mouvements anormaux. Ceci est également important pour dépister la possibilité de frottements oculaires nocturnes.
Bonsoir Docteur,
On m’a diagnostiqué un kératocône à l’œil gauche à l’âge de 15 ans. J’en ai 23 aujourd’hui.
Je ne me frotte plus les yeux depuis et mon kératocône parait stable.
Par contre, depuis quelques temps, en me réveillant le matin je vois flou et dédoublé des deux yeux pendant plusieurs heures. Je dois avouer que je suis parfois paniquée en me réveillant et en constatant que ma vue a drôlement baissé depuis la veille surtout que ça peut durer toute la matinée.( Impossible de lire, de travailler ou de conduire)
Qu’en pensez-vous? Dois-je m’inquiéter?
En vous remerciant par avance.
Mon keratocone n’évolue pas et au stade 1 mais j’ai des aberrations optiques de haut degré, comment c’est possible ? Ma vue était normale, les aberrations évoluent mais quand je fais des topographies, aucune évolution du keratocone constatée, je ne me frotte pas les yeux ni rien.. quelle est la solution selon vous docteur?
Si votre vision en binoculaire ne vous pose pas de particulier, il n’y a aucune urgence à réaliser une greffe de cornée.
Bonjour Docteur,
Je suis atteint d’un keratocone bilatéral, l’oeil gauche est presque épargné et ke keratocone est stable en revanche le keratocone de l’œil droit est au stade 4 car il a été détecté très tard mais il s’est stabilisé.
Je me suis finalement habitué à cette vue. On ne préconise de réaliser une greffe de cornée mais j’hésite encore.
Qu’en pensez-vous docteur?!
Merci beaucoup par avance.
Bonjour Dr Gatinel,
Atteint d’un keratocone stade 1 œil droit, le médecin me propose de faire un CXL, j’ai refusé, je ne me frotte jamais les yeux, je dors pas sur mon ventre pour éviter la pression sur mon œil. Pourtant les éblouissements et halos lumineux deviennent de plus en plus intenses et pas le contraire, maintenant la nuit je galère beaucoup avec la lumière de rue et les phares de voiture tellement les lumières sont dispersées de partout et sont comme des étoiles. Je veux savoir est-ce que cela explique l’évolution du keratocone ? Malgré le fait que je ne me frotte jamais les yeux et même durant mon sommeil, je mets un masque protecteur exprès pour ne pas me frotter les yeux. Est-ce que ces symptômes peuvent être traités ? Et est ce que cela ne veut pas dire réellement que le KC a évolué ? Merci d’avance docteur.
Bonjour Docteur,
Jai vraiment besoin de votre avis.
Jai un keratocone bilatéral diagnostiqué il y a 1an aujourd’hui je sors de mon rdv de contrôle et il se trouve que mon kc est stable malgré cette bonne nouvelle on m’annonce que mon astigmatisme a augmenté de 0.5 à chaque oeil (en un an) je suis donc a 2 et 2.25, mon ophtalmo me dit que cest dû à l’âge (je nai que dix neuf ans) et me laisse sur cette fin. Je ne me frotte plus et dors sur le dos.
Pouvez vous m’éclairer svp je suis inquiet.
Merci
Bonjour dr
J’étais diagnostiqué depuis 2 mois par un keratocone bilateral mon ophtalmologue a prescrit cross linking cxl pour mon oeil droit et je dois faire pour l’oeil gauche apres 1 mois. Mon question est ce que cross linking est dangereux ou bien elle ne doit pas etre réalisé ? Je lis une artcile que la cxl ameliore la vision chez 60 % des patients après 2 ans.
Et je lis vos articles que la maladie n’est pas d’orgine génétique mais il ya un nombre (moi, mon frere, mes cousins) des membres de nos famille qui est atteigne du keratocone.
J’espère que vous me répondez. Merci
Bonjour Docteur,
Merci beaucoup pour votre réponse!
Si vous me le permettez plusieurs questions me viennent encore:
1) Avant d’entreprendre une adaptation en lentilles rigides (qui sont réputées gênantes), j’aurais voulu savoir si dans mon cas (kératocône unilatéral), elles m’apporteraient réellement un meilleur confort visuel et une moindre fatigue oculaire?
En effet, améliorer ma vision de l’oeil gauche améliorera t-il ma vision binoculaire ou pas forcément dans la mesure où c’est l’oeil droit qui compense?
Voici ma correction:
OD: -4,25 (-1 à 90°)
OG: -5,75 (-3,50 à 100°)
2 ) Est-ce que ça fatigue mon oeil droit de compenser la mauvaise vision de mon oeil gauche et cela peut-il engendrer une fatigue visuelle ou un déséquilibre en vision binoculaire?
Désolé pour toutes ces questions;)
Encore Merci!!
Le port de lentilles rigide n’aggrave pas le kératocône; si vous les manipulez et les posez normalement, sans frotter les yeux après le retrait par exemple… ce qui est dommageable pour la cornée est la réalisation de frottements répétés, comme votre histoire clinique (et des milliers d’autres) le met bien en lumière. Dormir sur le ventre ou le côté est un facteur de risque, peut être pas en lui même, mais parce qu’il est difficile d’éliminer la présence de frottements nocturnes inconscients, dans la mesure où ce type de position induit généralement une irritation oculaire et des tissus adjacents. Cependant, la compression prolongée du globe oculaire n’est pas non plus souhaitable: risques non seulement cornéens mais internes (augmentation de la pression intraoculaire, mauvaise pour le nerf optique).
Bonsoir Docteur,
Merci beaucoup pour votre site web très enrichissant! Vous nous aidez à y voir plus clair:)
Si ça ne vous dérange pas, j’aurais quelques questions à vous poser:
1) j’ai un kératocône unilatéral à l’oeil gauche diagnostiqué lorsque j’avais 16 ans. Je ne me frotte plus les yeux depuis. Par contre, j’ai toujours beaucoup de mal à changer ma position de sommeil. Ma question est donc la suivante: Dormir sur le ventre ou sur le côté est-il suffisant pour aggraver le kératocône même si on ne se frotte plus les yeux? Dormir avec les yeux compressés comporte t-il un risque en soi mise à part le processus indirect qui est que cette position puisse donner davantage envie de frotter?
2) En vision monoculaire (avec correction), je vois bien de l’oeil droit mais flou et dédoublé de l’oeil gauche. En vision binoculaire je vois plus ou mois bien sauf la nuit ou dans les milieux sombres où j’ai plus de mal. Je fatigue vite quand je lis. Je porte actuellement des lunettes. Pensez- vous que j’aurai moins de fatigue visuelle et que je verrai mieux si je porte des lentilles rigides ? (Je suis étudiante et je travaille beaucoup sur ordinateur) ou bien que cela ne va pas changer mon confort visuel vu qu’il s’agit d’un kératocône unilatéral et que je peux compenser en vision binoculaire par mon oeil droit?
3) Est-il préférable que je reste en lunettes le plus longtemps possible? N’y a t-il pas un risque même faible que les lentilles puissent aggraver le kératocône par exemple par des manières inadaptées de pose et dépose des lentilles qui feraient que mon doigt rentre en contact avec mon oeil?
Merci beaucoup pour le temps que vous accorderez à me répondre.
Dans la grande majorité des cas, ces symptômes sont liés à une légère déformation de la cornée, qui est consécutive aux frottements (récents ou anciens), qui peuvent être effectués de manière plus ou moins consciente, parfois pendant la nuit. Il est important de réaliser un examen de topographie cornéenne (au moins) et une aberrométrie pour confirmer cela.
La dilatation de la pupille, quand il fait sombre, majore l’impact de la déformation cornéenne (kératocône) sur votre vision. La piscine n’a pas d’impact, et le CXL ne permet pas d’améliorer la vision (au contraire bien souvent, au moins transitoirement). En pratiquant certains sports comme la natation, il est important d’éviter de se frotter les yeux pour évacuer de l’eau ou les sécher.
Bonjour docteur,
Je suis atteint de keratocone, le matin je vois bien mais le soir j’ai beaucoup d’éblouissements, je vois des étoiles à la place des lumières qui m’empêchent de conduire la nuit. J’ai refusé de faire le CXL. Hier je suis parti à la piscine, quand la nuit est arrivée, les éblouissements sont devenus très forts et les traits d’éblouissements sont devenus plus nombreux et plus longs, est ce que c’est dû à la piscine et c’est temporaire ou c’est une évolution du keratocone ?
Je souhaite témoigner que je possède depuis avril 2023 les mêmes symptômes que Boubacar et Hugo, c’est à dire principalement:
– Des textes blanc sur fond noir qui bavent verticalement, avec parfois plusieurs réplications
– Plus généralement toute lumière brillante sur fond noir va créer une deuxième ou troisième image (Diplopie monoculaire)
– J’ai consulté 2 ophtalmo qui n’ont pas réussi à endiguer cette double image.
– Le test traditionnel des lettres noires sur fond gris en cabinet d’ophtalmologie ne permet pas de détecter les deuxiemes images car le contraste et la luminosité sont insuffisantes.
L’ophtalmologue m’a prescrit des lunettes qui n’aident absolument pas l’effet de double image.
Par ailleurs je voudrais ajouter les choses suivantes:
J’ai lu le témoignage de multiples personnes qui ont ce symptôme de double image monoculaire, mais les ophtalmologues semblent peu sensibilisés à ce problème et nous donne aucune solution en lien avec notre problème.
Est-ce un problème nouveau ?
Est-ce un problème davantage repéré par la prévalence des écrans ?
Existe-t-il des cabinets d’ophtalmologie qui proposent un test autre que le test typique de lettre noires sur fond gris ?
Pour ma part, je ne me gratte pas les yeux, en revanche je dors systématiquement sur le côté.
La meilleure technique est certainement de tirer la peau sur le coté, car il convient d’éviter d’appuyer sur les cornées. Les lavages au sérum physiologique réguliers sont indiqués pour ôter les allergènes et les irritants de la surface oculaire, et réduire ainsi l’envie de se frotter les yeux.
Bonjour.
Je suis atteinte d’un kératocone bilatérale en adaptation a des lentilles rigides… Sur les ordinateurs ou la nuit c’est très compliqué je n’arrive pas lire correctement avec. J’ai les yeux qui fatiguent et me démange beaucoup plus. Je me sens mieux avec les lunettes, je ne vois pas si mal avec. Dois je persévérer ?
Autre question pour éviter le frottement des yeux je pose un doigt sur l’oeil fermé dans pression et bouge l’oeil en dessous. C’est ok ça se rapproche d’un frottement ?
Où j’etire la peau à côté de l’oeil sur les côtés.
Je ne voudrais pas aggraver mon kératocone mais malgré les gouttes ce n’est pas facile.
Merci pour votre temps et votre aide
S’il existe une différence importante de correction entre les deux yeux, ou un fort astigmatisme, la correction en lunettes est effectivement impossible ou peu efficace (et mal tolérée).
A priori les forces mises en je sont trop faibles pour générer un stress mécanique cornéen significatif – contrairement à celles que représentent les frottements réalisés avec les doigts.
Bonjour docteur,
Est ce que fermer ou cligner fortement des yeux peut aggravée le keratocone ?
Merci pour vos travaux
Bonjour docteur,
Est ce que fermer fortement les yeux peut aggravée le keratocone ?
Bonjour docteur,
Est ce que cligner des yeux ou les fermer fortement peut aggravée le keratocone ?
Bonsoir je viens vers vous pour m’aidez,j’habite en martinique, ma fille a un keratocone diagnostiqué depuis 5 ans .elle porte des lentilles rigides, depuis 5 ans je demande a l’ophtalmologiste de nous prescrire des lunettes pour la maison ( télé…) elle me les refuse prétextant qu’elles sont inutiles. Je voudrais votre avis.je vous avoue que porter des lentilles toute la journée lui fatigue les yeux. Si minime que soit les lunettes l’aideraientdans ses petites tâches quotidiennes à la maison.Donnez moi votre avis .Merci
Vous pourriez également essayer l’adaptation d’une lentille sclérale, de large diamètre (que l’on remplit de sérum physiologique avant la pose). Ce type de lentille est plus stable que les lentilles rigides « mobiles », de plus faible diamètre.
Bonjour,
J’ai un kératocône très avancé à un de mes yeux. La cornée est très déformée et forme un pic avec une partie au centre qui est donc plus mince. On évalue ma vue à 1/10, voire moins tellement elle est floue avec cet oeil. L’autre a un kératocône aussi, mais très léger avec une vue évaluée encore à 10/10. On me conseille une greffe de la cornée pour l’oeil avec le kératocône très avancé, après avoir essayé des lentilles rigides 2-3 minutes avec un adaptateur de lentilles. Ce fût difficile de trouver une lentille pouvant tenir sur l’oeil, mais il y en a une qui a quand même tenu et je l’ai gardé 1 à 2 min.
Je me demandais si la greffe était la seule solution dans mon cas et au bout de combien de temps (d’adaptation ou d’essai) on peut considérer que des lentilles ne peuvent plus être une solution.
Merci d’avance pour votre réponse et toutes les informations sur votre site web.
La pose d’anneaux est réservée aux cas où il existe un astigmatisme prononcé et une déformation avérée. Les anneaux permettent de réduire l’irrégularité de la déformation mais peuvent également induire certaines perturbations visuelles. Si votre kératocône est unilatéral (frottements très prédominant d’un côté) il est important de vérifier que vous n’ayez pas une position de sommeil impliquant une compression prolongée de l’oeil gauche (position sur le ventre ou le côté avec appui de la tête du côté gauche). Les lunettes ne corrigent pas les déformation aymétriques qui induisent les images fantomes décalées vers le bas. Les lentilles rigides procurent la meilleure correction possible pour le kératocône; certains patients observent parfois une inversion de la direction des symptômes visuels (petit décalage résiduel vers le haut). Ceci est lié à la face postérieure de la cornée, dont la déformation n’est pas corrigée par la lentille (située à la face avant de la cornée).
Il convient dans un premier temps de réaliser un examen de topographie cornéenne, afin de vérifier qu’il n’y ait pas d’astigmatisme irrégulier, qui s’observe en général quand on se frotte trop souvent les yeux; ces frottements provoquent de légères déformations de la cornée, et sont à l’origine de la majorité des symptômes visuels tels que ceux que vous décrivez. Quand les frottements continuent, les déformations s »accentuent et un aspect de kératocône peut être observé.
Bonjour Docteur,
J’ai 21 ans. Depuis décembre 2022, j’ai quelques petits soucis.Tout a commencé par une sensation de fatigue aux yeux et un petit flou de loin et après J’ai eu les lumières qui bavent vers le haut et énormément (2-3m) à partir de 150 mètres. il y a aussi des stries qui vont vers le bas et des éclairs partout autour de la source lumineuse. Ajouté à cela un trait oblique qui traverse la source lumineuse, je peux dire que je ne peux plus conduire de nuit. Aussi j’ai un dédoublement parfait vers le haut de tout ce qui est écriture sur fond noir quand c’est de près, et de loin tout ce qui est écrit et lumineux (comme le numéro de ligne d’un bus) apparaît aussi en double. Il arrive d’observer une vision triple (un dédoublement très léger vers le bas) selon les angles.
J’ai consulté plusieurs ophtalmos. Le premier en décembre m’a diagnostiqué un petit astigmatisme -0.5 aux deux yeux et une petite myopie à l’œil droit (-0.25), accompagné d’un défaut de convergence. J’ai fait un fond d’œil et résultat une excavation papillaire à 0.35 à contrôler dans 1 an (qui n’a rien de grave d’après l’ophtalmo). Donc j’ai fait 5 séances de rééducation avant d’arrêter par manque de temps et aussi l’orthoptiste qui me disait que j’allais bien et que mon problème n’est pas un problème orthoptique. Les lunettes que j’ai eues me rendaient la vue (vraiment) plus nette mais les dédoublements et les problèmes de lumière n’ont pas été résolus.
Une deuxième ophtalmologue m’a dit que je n’étais pas du tout myope mais hypermétrope (+0.25 OD, +0.5 OG) et aussi que mon astigmatisme à évolué à l’œil droit à augmenté (-0.75). Le problème n’est toujours pas résolu et le pire c’est que je vois moins bien de loin avec ces lunettes.
Un troisième ophtalmo m’a quasiment fait les mêmes mesures en me disant que je n’étais pas du tout myope.
Dernièrement on m’a refait des lunettes avec +0.50 ajouté à chaque œil donc +1.0 OG +0.75 OD avec la même correction astigmatisme. C’est encore pire de loin, les lumières sont encore pires. J’ai à nouveau fait un fond d’œil qui n’a pas trouvé quelque chose d’anormal et l’ophtalmologue m’a dit que tout est normal cette fois et l’excavation papillaire est normale pour le type papille que j’ai.
J’ai toujours dit aux 3 derniers ophtalmologues que je vois mieux avec les lunettes pour myope mais ils persistent tous et disent que je suis pas du tout myope et me font une correction hypermétrope qui me fatigue les yeux et qui rendent ma vision brouillée de loin.
Donc voilà je suis vraiment dans le désarroi, je sens que les problèmes avec les lumières s’aggravent car j’ai plus de bizarreries autour des lumières qu’avant et j’ai toujours pas de piste de solution. Merci et désolé si je vous ai perdu dans mes explications
Bonjour.
J’ai 30 ans, et j’ai consulté un ophtalmologue ce mois car depuis plusieurs mois j’avais un dédoublement vers le bas de lumière sur fonds noir. Les Phares la nuit, ou panneaux lumineux etc…
L’ophtalmologue m’a indiqué un keratocone à l’oeil gauche, et un oeil droit sain.
Il m’a dit d’arrêter de me frotter les yeux, et qu’un cross liking était inutile si arret des frottements. Son conseil converge avec le votre ce qui est rassurant.
Je dois retourner le voir dans 6 mois. J’ai une nouvelle paire de lunettes car mon astigmatisme à légèrement augmenté..
Cependant j’ai toujours le dédoublement vers le bas des objets lumineux le soir. Est ce que la pose d’anneaux pourrait régler ce problème en redonnant une bonne forme à ma cornée ?
Porter des lunettes ne me dérange pas du tout. J’ai juste peur de ne pas supporter des lentilles rigides…
Merci d’avance
Ceci est possible, en fonction de la dilatation de la pupille, de l’étalement des larmes, de certains facteurs subjectifs, etc.
Il convient de répéter les examens topographiques et faire des cartes différentielles: parfois, les petites « évolutions » peuvent correspondre à des régularisations épithéliales, consécutives à l’arrêt des frottements.
Bonsoir Dr,
Lors de mon rdv pour suivre une eventuelle evolution de mes kc, on m’a dit qu’un oeil n’avait pas evoluer mais que l’autre avait eu une petite evolution. Sachant que je suis assez jeune j’ai donc conscience que ca peu evoluer rapidement je ne me frotte plus du tout les yeux et je dors sur le dos, pour vous dire je n’arrive meme pas a me netoyer les paupieres et autours des yeux correctement alors qu’ils se salissent assez vite.
Pouvez m’en donner une explication docteur?
Merci d’avance
Bonjour docteur,
Est-ii possible d’avoir une augmentation des symptomes du keratocone ( dedoublement d’image brillante sur fond noir) alors que la refraction et la topologie ne revelent pas de progression de keratocone?
L’arrêt des frottements et la protection de vos yeux la nuit sont les éléments les plus importants pour garantir l’absence d’évolution de la déformation de vos cornée, qui paraît relativement modérée au vu des corrections en lunettes (en cas de kératocône plus évolué, on observe généralement un fort astimgmatisme myopique). Il est fréquent que les lentilles rigides ou les lentilles sclérales occasionnent la perception de symptômes visuels dont l’orientation est opposée à celle qui sont perçus en correction lunette. Ceci est lié au fait que les lentilles ne corrigent « que » les aberrations optiques de la face avant de la cornée. Elles « démasquent » ainsi les aberrations de la face arrière, qui ont un pattern opposé pour des raisons optiques (variation d’indice de réfraction de signe opposé au contact de la face postérieure avec l’humeur aqueuse qui baigne la chambre antérieure de l’oeil. Il n’y a pas de technique chiurgicale à même de faire mieux que les lentilles rigides. Si vous ne frottez plus vos yeux, votre vision demeurera stable.
Bonjour Dr.Gatinel, y a-t-il une corrélation entre les aberrations optiques de haut degré et la correction en lunettes ? Je vous explique mon cas j’ai 25 ans j’ai découvert mon keratocone bilatérale stade 1 il y’a 5 mois et arrêté tout frottement et changer de position de sommeil accompagné de coque de protection depuis. Correction en lunettes : OG +0.25 (+0.25) ET OD -0.25 (+1.00) . Et il y’a eu aucune évolution entre les 2 topographie (5 mois) OG kmax 43.8 pachy 484 et OD Kmax 44.9 pachy 478.
J’ai des aberrations optiques de haut de degrés qui apparaissent la nuit ou dans une pièce très sombre (feu et led qui bavent ou se dédouble etc..) et dans les 5 mois c’est aberrations ont quasiment doublé sans que ma correction ai changé ou que les résultats topographiques montre une évolution.
Je vous donne un exemple très détaillé la nuit un feu rouge a 400 metres bave de 2 mètres vers le bas et j’ai essayé les lentilles sclérales et semi rigides mais les feux bavent vers le haut avec la vision légèrement floue et un petit arc en ciel de couleur au bout, du coup je ne sais pas si la lentille est vraiment une solution pour mon cas et c’est pour sa que je sollicite votre aide pour dans un premier chercher a savoir le facteur qui aggrave les aberrations optiques de haut degrés et ce qui peut réduire ces aberrations en plus des lentilles ( chirurgie ou autre ) . Je m’investis beaucoup pour stabiliser le keratocone et traiter ma vision de nuit car je souhaite garder mon travail dans la conduite des trains et que si sa évolue je serai dans l’obligation d’arrêter définitivement.
Merci d’avance.
Merci pour votre témoignage qui rejoint la réalité du keratocône qui est évidemment une pathologie d’origine mécanique. Arrêter les frottements enraye la progression, continuer soumet la cornée à un stress répété responsable de la déformation et de l’amincissement qui s’accentuent au fil du temps. Contrairement à ce qu’on lit parfois, la cornée ne semble pas durcir avec l’âge et si elle le faisait, ce ne serait pas suffisant pour devenir invulnérable vis à vis des frottements. Dans mon expérience, dormir sur un oeil n’est pas conseillé, mais cela ne semble pas être suffisant pour provoquer l’apparition de ce que l’on appelle keratocône (amincissement central avec déformation permanente). Toutefois, ce type de position de sommeil est propice à l’induction d’une irritation oculaire chronique, elle même source d’une envie de frotter. En définitive, si vous ne frottez plus du tout, vos cornées resteront en l’état.
Bonjour Docteur,
Je reviens vers vous après 6 ans pour d’abord vous remercier du plus profond de mon cœur car depuis que j’ai arrêté de me frotter vigoureusement les yeux (je le faisais a l’aide des phalanges) mon keratocone n’a pas du tout évolué .
Je vis avec des lunettes et ma vue est de 10/10.
Grâce à vos conseils il n’a pas évolué.
J’ai maintenant 35 ans, est il vrai que la cornée a tendance à se rigidifier après 30 ans et donc stoppe l’évolution du keratocone ?
Autre question : je dors la tête enfouie dans l’oreiller l’œil appuyant sur l’oreiller avec une pression sur l’œil, est ce que ce comportement seul peut aggraver le keratocone sachant que je ne me frotte JAMAIS les yeux ?
Merci à tous de partager cette merveilleuse lumière à ceux qui ont besoin d’une aide urgente, cette opportunité est vraiment formidable. Je veux également partager cette incroyable critique avec le monde sur ce grand médecin traditionnel africain appelé Dr SANI, qui a aidé à guérir mon virus de l’herpès de 18 mois avec ses puissants médicaments à base de plantes, j’ai souffert d’herpès génital pendant 18 mois, pendant cette période j’ai visité plusieurs hôpitaux et utilisé plusieurs médicaments, mais il n’y avait pas de solution jusqu’à ce que je tombe sur le site Web du Dr SANI en cherchant de l’aide. J’ai trouvé tellement de critiques incroyables sur lui et sur la façon dont il a guéri tant de personnes dans le monde avec ses plantes médicinales, j’ai décidé de lui donner une chance de m’aider à guérir mon virus de l’herpès aussi et j’ai contacté son e-mail : (PERFECTHERBALCURE@GMAIL. COM) J’ai expliqué ce que je traversais, il m’a donné de l’espoir et m’a assuré que je serai guéri et sauvé de mon herpès génital avec ses médicaments. J’ai suivi ses instructions et il m’a envoyé de puissants médicaments à base de plantes via le service de messagerie, que j’ai pris pendant 2 semaines et mon herpès a disparu et j’ai été complètement guéri. Je suis tellement heureuse de cette belle expérience, cela fait des mois que je suis guérie et je n’ai plus revu aucun signe ou symptôme du virus, pas même les épidémies habituelles.
Dans le cas où vous auriez la même maladie, je vous conseillerai d’aller directement voir ce grand homme par Email : perfectherbalcure@gmail.com OU Appelez-le/WhatsApp au : +2348118184266
Il ne faut pas vous inquiéter outre mesure, car la position de sommeil seule ne suffit pas à induire un kératocone en l’absence de frottements. Réalisez dans un premier temps une topographie cornéenne, et essayez de modifier votre position de sommeil : le port d’une coque n’est nécessaire qu’en cas de frottements et kératocône avéré. On en trouve en pharmacie, ou sur internet.
Bonjour docteur,
Je suis étudiant, je travaille donc beaucoup sur ordinateur, j’ai 23 ans et j’ai une myopie faible (-2) associé à un astigmatisme (faible aussi pour l’instant inférieur à 1) sur les deux yeux. Je soupçonne depuis peu d’être atteint d’un kératocône et j’en suis relativement anxieux comptant réaliser une opération pkr ou lasik dans les années à venir.
En effet, je remarque que je présente plusieurs symptômes: je dors depuis des années sur le ventre, j’ai une vision floue au réveil pendant 2 à 3 minutes, j’ai du mal à m’habituer aux lentilles/lunettes et également mon astigmatisme qui était néant lors de ma première consultation ophtalmologie à 18 ans est désormais de 0.5 à droite et quasiment 1 à gauche. Jusqu’à maintenant, je me pensais à l’abri et j’ai toujours évité de me frotter les yeux mais je n’avais jamais pensé à la position de sommeil et d’apprendre cela me fait assez peur. En attendant ma consultation chez mon ophtalmo où je vais demander une topographie cornéenne, auriez-vous des conseils quand à l’achat d’une éventuelle coque oculaire pour protéger mes yeux la nuit ou d’autres conseils de prévention?
Merci beaucoup
FG
Le kératocône n’est pas une maladie primitivement génétique comme on a pu vous le raconter, mais la conséquence de frottements oculaires répétés avec les phalanges, les poings, etc. Les impacts indirects de coups portés à la tête n’ont aucun effet sur la cornée et le kératocône. En revanche, si vous transpirez au cours des séances d’entrainement, et vous essuyez les yeux vigoureusement, alors vous pourriez induire une progression de la déformation, mais cela est vrai quel que soit le sport: boxe, tennis, patinage, foot, natation, etc. Si vous pouvez combattre sans porter de lentilles, il n’y a pas de problème a redouter. Si vous devez porter des lentilles rigides, celle-ci peuvent en revanche poser des soucis (déplacement). Les lentilles sclérales sont plus stables. En conclusion, si vous pouvez réaliser votre sport sans correction optique, il n’y a pas de souci, évitez simplement de vous frotter les yeux.
Bonjour Docteur,
Je suis un jeune boxeur de 20 ans, la boxe c’est toute ma vie mais je suis atteint d’un kératocône me contre indiquant à la boxe en compétition.
Le 26 mars 2016 vous avez écrit en réponse à un commentaire : « La pratique de la boxe et des sports de combats est possible en cas de kératocône »
Cette phrase est-elle aussi vraie pour la pratique de la boxe en compétition ? Y’a-t-il une solution pour moi ou je serai toujours contre indiqué de boxe en compétition même en cas de traitement par crosslinking ? Les lentilles sclérales peuvent elles changer la donne ?
Merci d’avance pour votre retour.
Bonjour docteur gatinel,
Avez vous deja entendu parler du docteur gulani c’est un docteur des etats unis et apparamment cest le seul qui sait guérir le kc grâce aux techniques qu’il a inventé lui même comme le Lazrplastique on peut constater sur la chaine youtube gulani vision de nombreux témoignages de patient atteint de kc traiter par ce docteur et qui on récupèrer une vision de 20/20 sans lunettes ni lentilles, il explique lui même dans certaines vidéos ses techniques et comment il procéde.
Qu’en pensez vous pourrait ton avoir les mêmes traitements en france?
Le kératocône est provoqué par la réalisation de frottements oculaires excessifs répétés, et non par une infection oculaire bien entendu.
Il est important de veiller à ne pas appuyer sur les globes oculaires lors des massages. Dans ma pratique j’ai observé au moins deux cas de kératocône induits par des frottements excessifs pour hygiène des paupières: les patients frottaient les paupières vigoureusement et plusieurs fois par jour. Si vous effectuez les massages correctement et comme indiqué, il n’y a pas de risques.
Bonjour Dr j’ai un DGM , je dois faire des messages quotidiens des paupières supérieures et inférieures. y a t’il un risque de développer un Kc ( frottements quotidiens finalement)
merci
bonjour docteur Gatinel
que pensez vous des affirmations d’un certain ophtalmogue en Italie qui affirme que le kératocone est infectieux (champignon) et qu’il a trouvé les techniques pour le guérir définitivement je suis moi même atteinte de kératocône avec un suivi régulier et greffée
merci et bonne journée
Bonjour
je lis « par hasard » et avec grand intérêt votre article après un rendez vous à Paris pour mon suivi de kératocône. Je ne suis pas médecin mais il y a des logiques de causes à effet à relier, c’est bien dommage que les médecins pour la plupart ne cherchent pas dans une globalité et s’arrêtent à leur domaine. Pour ma part, j’ai 36 ans, j’ai été diagnostiquée avec un kératocône vers 2008 environ. Juste après avoir eu comme diagnostic une rosacée oculaire. peut être deux ou trois ans avant tout cela j’avais été opérée des amygdales à cause d’angines à répétition notamment à staphylocoques dues à un écoulement nasal inverse et constant (que j’ai toujours!). Il y a un fort terrain allergique du côté maternel.
Les tests de base d’allergie n’ont rien donné, comme j’avais 20 ans et que sinon j’étais en pleine forme je me suis faites souvent agressée par des médecins qui ne comprenaient pas pourquoi « je cherchais à avoir quelque chose » je cite.
J’ai encore récemment été voir un orl qui m’a dit qu’il n’y avait rien de grave qu’il faut vivre avec la cause n’est pas connue.
Puis à commencé des conjonctivites à répétition (1par mois), un medecin généraliste m’a même prescrit de la crème musculaire camphrée à mettre sur mes paupières, un opthalmologiste m’a ensuite soignée de cette catastrophe mais m’a ensuite prescrit des corticoides en gouttes durant 2ans sans savoir ce que je pouvais bien avoir puis à paris j’ai eu le diagnostique de rosacée oculaire. J’ai ensuite eu des crises d’herpès oculaire (cela fait 10 ans que je n’ai pas refait de crise) puis l’on m’ a diagnostiqué un kératocône 6 mois après. Celui ci evoluait jusqu’au jour ou le professeur que j’allais voir m’ a dit que les massages pour la rosacée (qu’il m’avait prescrit) ne faisaient qu’aggraver l’évolution du kératocône mais qu ‘ a part bien relever ou baisser les yeux en fonction du massage pour la rosacée je favoriserai le kératocône mais que « c’était comme ça » que tout frottement en dormant sur ses phalanges ou en se frottant les yeux aggravaient la situation, dommage de ne pas l’avoir su dès le départ. Je me suis astreinte pour ma rosacee à presque me révulser les yeux à l’inverse des mouvements de massage quotidiens de ma rosacée, à penser à ne pas m’endormir sur mes phalanges et à essayer de ne plus dormir sur le ventre. Résultat mon kératocône en 12 ans a très peu évolué, quasiment pas. J’essaie de parler de cette allergie qui fait que j’ai les cornets gonflés constamment car je reste persuadée qu’elle est la cause du reste mais le corps médical ne m’écoute pas. Mais peut être est ce aussi le symptome premier d’autre chose (dérèglement de la flore intestinale? Polluant pas encore étudié dans les tests allergiques?). Je précise que du coté maternel il y a sur cette branche de l’asthme, de l’eczema et chez les femmes des problèmes de thyroide de hashimoto. du côté de mon père celui ci a eu récemment une leucemie aigue et s’en ai sorti grace à une greffe de cellules souches d’un donneur il me semble que cette leucemie resulte d’une défaillance d’un gène je ne me rappelle plus lequel. Cependant à part ça nous avons plutôt une santé de fer. Ma soeur est elle myope et astigmate avec un kératocône frustre. Je ne sais pas si cela peut vous être utile d’avoir mon temoignage mais pour une fois que l’on peut exprimer son ressenti et son avis sur son propre corps sans être recadré par la « science » du médecin qui ne souhaite pas notre avis sur nous même puisqu’on a pas fait medecine alors je ne m’en prive pas :) je vous remercie pour vos recherches et votre article.
Bonjour jai le keratocon et ce que je peux faire une correction lazer
Bonjour Docteur, pensez-vous que le fait de faire des attractions fortes (avec forte accélération, looping etc) puisse aggraver le keratocone ? En dehors du fait de se frotter les yeux, je me demande si un choc à oeil (tel que celui qu’on peut avoir dans ce genre d’attraction lorsqu’on démarre vite par exemple) ne pourrait pas avoir un impact négatif ?
Merci
L’évolution du kératocône est posée sur la topographie cornéenne, pas sur des impressions visuelles, qui peuvent être liées à des paramètres comme la sécheresse oculaire, l’état accommodatif, le diamètre pupillaire, etc. Si vous avez « sanctuarisé » les yeux, vous ne progresserez pas. Je vous invite à bien hydrater les yeux au cours de la journée, et faire des pauses régulières.
Il est difficile de vous donner des explications tangibles sans examen détaillé avec est sans les lentilles sclérales; je vous conseille de revoir votre praticien adaptateur pour éclaircir ce point.
Bonjour docteur, je suis âgé de 23 ans . Cela fait pratiquement 5 années que ma vue à commencé par baisser de mal en pire . J’ai d’abord été équipé en lunettes de vue et ensuite en lentilles RGP ( après un CXL sur l’oeil gauche ) actuellement ça fait une semaine que je suis équipé en Lentilles sclérales.
Mon problème est j’ai un petit flou blanc qui apparaît quelques minutes après le port des lentilles . Est-ce du au fait que mes lentilles ait mal été prescrites ?
Aussi ma vue n’est pas terrible avec les lentilles portés alors je me demande si j’essayais de porter des lunettes par dessus les lentilles , est ce recommandé et ma vue s’améliorera t’elle ainsi ?
Bonjour Docteur,
Je vis avec un keratocone bilateral depuis 24ans.
Decouvert en 1998 avec port de lunette pendant 2 ans puis vite equipée en lentilles de contact. J’ai eu un cross linking sur les 2 yeux en 2008/2009 puis ensuite un equipement en piggy pack jusqu’en 2021 (avec secheresse oculaire je mettais toujours des gouttes artelac pour les supporter toute une journee). Depuis 2021 le keratocone ne fait que évoluer (je ne me frotte plus les yeux depuis longtemps) jai depuis 1 an des lentilles sclerales, (que je supporte bien) et avec lesquelles mon accuité visuel peut aller a 8/10 sauf que en 10mois je suis redescendu a 6/10. J’ai des opacités sur l’oeil droit depuis 2ans, et actuellement suite a de nouvelles erosions et rupture de la couche de Bowman un traitement de vitamine A a mettre dans les 2 yeux (jai egalement des gouttes Vismed a mettre matin et soir depuis plusieurs mois pour la secheresse oculaire).Mon quotidien devient difficile car je travail sur ordinateur 8h/jrs, je souffre de migraines, de douleurs dans les yeux, la conduite de nuit devient difficile, et la vue se degrade rapidement une fois avec une nouvelle adaptation de lentilles….ma vue est souvent dedoublée notamment de loin ou je peut voir des silhouettes mais pas les traits d’un visage. Ma question est pourquoi depuis 24ans le keratocone evolue de facon recurente ? Puis je continuer a travailler sur ordinateur ? Pourquoi a mon stade qu’on le dit avancé n’y a t’il pas de solution de proposée comme une greffe ? En vous remerciant par avance de vos conseils. Bien Cordialement.
Bonjour Dr , j’ai une question ayant un keratocone non traiter par des lunettes ni lentilles ça me gêne la vision plus qu’autre chose) . J’ai remarquer que lorsque je reste devant des écrans pendant très longtemps (8h-9h par jours) mon keratocone évolue , est ce possible ? Je tien a préciser que je ne me gratte plus du tout les yeux , j’ai réussi a « sanctuariser Mes yeux » comme vous le dire si bien . Voilà comment cela se fait il que mon keratocone a l’air d’évoluer lorsque je reste beaucoup de temps devant les écrans (avec sûrement une bonne fatigue oculaire ) . Merci de votre réponse je cherche désespérément à stopper la progression de cette maladie .
Bonjour dr Gatinel,j’ai un Keratocone et je porte actuellement des lunettes avec laquelle je vois double et n’arrive pas à lire de près,comment puis-je corriger ce problème?Cordialement.
Cette technique existe déjà pour stabiliser le kératocône, et est extrêmement simple du moins à énoncer: il suffit de ne plus se frotter les yeux. L’existence d’un traumatisme mécanique répété est nécessaire pour induire la déformation et l’amincissement de la paroi de la cornée (qui définissent le kératocône). Je suis des centaines de patients qui ne progressent plus une fois l’éviction des frottements. En pratique, ceci n’est pas toujours facile à obtenir, en particulier chez les patients qui présentent une sévère atopie, ou encore ceux qui n’arrivent pas à contrôler ce geste (en particuleir la nuit). Guérir une fois que la déformation cornéenne est avérée n’est malheureusement pas possible en l’état actuel de connaissances. Il faudrait pouvoir réparer in situ les lésion générées par les forces de distention et les mécanismes biologiques associés, peut être un jour avec des nanotechnologies, des thérapies cellulaires ciblées, etc. En attendant, le kératocône pourrait être éradiqué ou du moins fortement réduit en incidence si le message clé (« no rub, no cone ») était porté à la connaissance de la population générale, ce que se site et son auteur s’évertue à faire. Malheureusement, cette approche ne sert pas certains intérêts et heurte un certain conservatisme et des idées préconcues sur le kératocône, qui sont difficiles à dissiper….
Bonjour DR,
Pensez vous que dans un futur proche il y aura une nouvelle technique pour stabiliser ou même guérir du keratocone??
Le plus important est effectivement de cesser les frottements, qui ont entrainé la déformation (heureusement légère dans votre cas). Si les gouttes ne vous paraissent pas efficaces et que vous ne vous frottez plus les yeux, alors il ne parait pas nécessaire de les poursuivre. Vous pourrez certainement corriger votre vision en lunettes – ou en lentilles dorénavant, mais si les frottements sont vraiment arrêtés pour toujours, il n’y a pas à redouter d’évolution. Le kératocône n’est pas une maladie génétique ou cornéenne primitive.
La greffe est une solution de dernier recours, qui est indiquée en cas d’astigmatisme et déformation extrême, et/ou d’opacités de la cornée. La précision de la correction apportée par une greffe est faible; elle induit souvent de la myopie résiduelle et de l’astigmatimse. Il existe des risques de rejets, le retrait des fils prend du temps,… Il est préférable de se corriger en lentilles rigides. Si vous ne frottez plus les yeux, aucune évolution significative n’est à redouter.
Bonjour docteur Garinel,
Je me posais la question concernant la greffe de cornée, j’ai un kc et peut etre que un jour je ferais une greffe de cornée pour me débarrasser de ce keratocone (même si je ne me frotte plus du tout les yeux j espere que ca n’évoluera pas). Alors ma question: est-ce en faisant une greffe de cornée on perd la myopie et l astigmatisme causé par le keratocone sachant que avant le keratocone je n’avais pas de problème de vue.
Merci pour ce que vous faites pour nous.
Bonjour
Mon fils a vécu un vent de sable dès l’âge de 4ans, après à été infecté par une allergie chronique jusqu’aujourdhui. Chaque fois un traitement ne sera pas efficace pour une autre fois et on changera un autre traitement. La plupart des avis des médecins est le même
Allergie des yeux il faut entretenir par un traitement jusqu’à l’âge de 18 ans et sappartira tout seul. Malheureusement ses yeux maintenant souffrent d’une baisse de vision
Au départ c’est une œil maintenant les deux
Je ne sais pas quoi faire
J’ai tout son dossier
Pouvez vous m’aider svp
Merci beaucoup
Bonjour docteur,
J’ai 18 ans et j’ai été diagnostiqué de kératocône récemment. Depuis le diagnostique je suis dépité. Suis-je condamné à avoir des problèmes de vision toute ma vie et donc ne plus pouvoir vivre comment avant? Mes keratocones sont débutants, mon docteure m’a prescris des gouttes anti allergie qu’elle appelle également anti demangeaison à mettre 3 fois par jour pendant 1 an mais quand je mets mes gouttes mes yeux me piquent et je dois mettre de l’eau pour apaiser les piquotement (je ne sais pas si c’est la transpiration qui entre également dans mes yeux qui entraine cet effet de picotement) j’ai l’impression que les gouttes ne me servent à rien car j’ai déjà appris à ne plus frotter mes yeux et mes yeux ne me démangent pas tant que ça, dois je ne plus en mettre ou réduire les 3 fois par jour à 1 ou 2 ?
Merci docteur d’avance.
La pression des paupières ou des cils est trop faible pour déformer le tissu cornéen, mais le frottement des cils peut endommager la surface de la cornée. Ceci peut en retour déclencher une sensation de gêne chronique, qui peut conduire à se frotter les yeux. Les manoeuvres délicates effectuées sur les yeux ne sont pas un risque pour provoquer ou accentuer le kératocône. Ce sont les frottements excessifs, prolongés, et répétés, avec les phalanges surtout.
Bonjour docteur,
Je suis atteint d’un kc sur les deux yeux.
J’ai arrêté les frottements oculaires mais j’ai tendance à avoir des cils qui rentre dans mes yeux, pour cela je mets juste de l’eau dessus et j’essaie de cligner plusieurs fois pour que le corp étranger parte. Ma question c’est est-ce que des cils qui rentre dans les yeux peuvent déformer la cornée et donc aggraver le keratocone? Pour enlever le chassie qu il y a sur mes yeux je mets également de l’eau dessus et j’essaie de les retirer tout doucement avec des compresses sans appuyé ni frotter dessus, cela n’aggrave egalement pas le keratocone n’est ce pas?
Merci d’avance pour votre reponse docteur.
Bonjour,
J’ai un keratocône à l’oeil gauche 1/10 et à l’oeil droit 12/10.
Connaissez vous des bons centres pour le kératocône (lentilles,suivi, chirurgie) dans le nord ouest de la France?
Car là où je vais : Institut Sourdille Atlantique j’ai un doute sur le suivi et la chirurgie (lentille ça va).
Merci
Cdt.
Il est possible que les frottements aient provoqué une légère déformation de vos cornées, mais si la magnitude de l’astigmatisme n’est que de 0.25, ceci est très rassurant et souligne que la déformation est très modérée. Un remodelage est possible (l’épithélium de la cornée peut régulariser au moins en partie la surface de la cornée). Les corps flottants sont possiblement liés au frottements; l’inspection de vidéos d’IRM dynamique montrant l’impact des frottements sur l’oeil révèle que non seulement la cornée, mais l’oeil dans son ensemble est vulnérable aux frottements: https://www.youtube.com/watch?v=tM4z3MYZeNk
Bonjour Docteur,
Je suis atteint d’un kératocône avancé et suite à une tentative d’adaptation en lentilles rigides échouée, je dois normalement être équipé en lentilles sclérales. D’après mes recherches et ce que me dit mon ophtalmologue, ces lentilles ne sont à la base pas destinée au kératocône (manque d’oxygène, etc). Je me pose donc la question sur l’impact possible de ces lentilles à long terme sur ma cornée. Vont-elles abîmer ma cornée? Vais-je de moins en moins bien les supporter?
J’ai une appréhension à tenter cette adaptation en sclérales car ma vision actuelle me permet encore de voir +/- bien grâce à mon œil gauche qui est à 8/10. Je me rends compte que ma vision n’est pas top (difficulté à distinguer des visages de loin, vision de loin pas terrible en règle générale) mais est-ce que le risque des sclérales en vaut le coup? J’ai en effet peur d’avoir une bonne amélioration avec les sclérales pendant 5/10 ans mais d’avoir un retour de baton par la suite et de passer au stade greffe…
Merci pour votre réponse!
Bonjour docteur
Je voulais savoir quelque chose, je suis sûrement atteint d’un keratacone debutant d’après les symptômes évoqués et il y a eu l’apparition d’un astigmatisme débutant à 0,25 aux 2 yeux, je voulais savoir sur le long voire très long therme avec l’arrêt complet de tout frottement si l’oeil , surtout la cornée possède la capacité à retrouver sa forme initiale. Des corps flottants ont fait leur apparition en même temps que mon début de keratacone , peut-être du à la désorganisation des fibres de collagène, J’espère qu’eux aussi partiront
La lentille sclérale est certainement le moyen le plus efficace pour améliorer la vision en cas de kératocône avancé. Le fait de dormir en appuyant sur l’oeil droit est certainement un facteur entrant dans le mécanisme ayant conduit à vous frotter cet oeil (ceci peut intervenir pendant la nuit de manière inconsciente, ou le matin au réveil). Il est conseillé de cesser ceci et porter des coques de protection oculaire à fixer avec du micropore (prescription) ou trouver un masque de protection oculaire suffisamment confortable pour qu’il n’empêche pas de bien dormir. La déformation ne s’accentuera pas si vous cessez tout frottement répété et ceci concerne non seulement le jour mais également la nuit. Le port des protections nocturnes a également valeur de test car nombre de patients se surprennent à frotter le masque pendant la nuit, ou signalent que celui ci se déplace ou se détache pendant la nuit – ceci traduit l’action de forces au niveau de la zone du visage et des yeux pendant la nuit.
Bonjour docteur,
On vient de me diagnostiquer un kératocone stade 4 sur mon oeil droit. Mon ophtalmologue m’a dit que pour l’instant elle ne pouvait me prescrire que le port d’une lentille sclérale pour améliorer ma vue. Je souhaitais savoir s’il y avait de bons résultats (sachant que c’est assez coûteux).
D’autre part, je ne me frottais pas particulièrement l’oeil mais je pense que mon keratocone s’est accentué car je dormais sur mon oeil droit. Aujourd’hui, j’ai dû mal à changer de position. Même avec toute me bonne volonté, je me réveille souvent sur un de mes yeux… Y aurait il des astuces ?
Enfin, à cause de la maladie, mon oeil droit a fini par loucher (ce qui était léger mais arrive de plus en plus). Je voulais savoir si ce strabisme pouvait s’attenuer (voir disparaitre) grâce aux traitements.
Cordialement
Bonjour
Confirmez-vous que seule la compression augmente le risque de keratocone ? En effet dormir sur le côté est possible si on prend soin de ne pas mettre l’oeil en contact directement avec un oreiller dur ou la main ?
Désolé pour la question bête
Lucie
Bonjour docteur , j’ai 18 ans et avant environ 3 mois aucun problème de vu. Je n’ai aucune idée de ce qu’il s’est passé au début mes yeux me piquaient très durement au contact de la lumière et les lampadaire feux tricolores petite lumière concentrée apparaissaient de manière floue et parfois dedoublés , ma vision a chuté légèrement de loin je suis donc allé voir un ophtalmo et m’a dit que j’étais devenu astigmate de façon très légère -0,25 et +0,25.Ensuite ma vision s’est amélioré au même niveau qu’avant sauf que les lumières apparaissent toujours floue et maintenant des corps flottants sont apparus en très grand nombre ainsi que des éléments que l’on peut assimiler à des flocons de neige tomber de mes yeux visible sur des fonds uniforme. Après un examen du fond d’oeil aucun diagnostic posé pour mes problèmes de vision voila j’espère que vous pourrez m’aider merci pour votre attention et votre temps
De nombreux traitements, remèdes ou solutions plus ou moins originales ont été proposées pour le kératocône; aucune n’est efficace sauf celle qui consiste à ne plus se frotter les yeux, et traiter toutes les causes qui peuvent conduire à trop se frotter les yeux. Le mécanisme conduisant au kératocône n’est pas intrinsèque mais extrinsèque (frottements oculaires excessifs).
Bonsoir Docteur
J’aimerais savoir si la prise des comprimes de gelatine et vitamine A pourrait aider les patients de keratocone sil vous plait?
MERCI D’AVANCE
En cas de kératocône avancé, les lentilles sont le meilleur moyen de récupérer une vision de qualité. En fonction de la déformation, des caractéristiques de l’oeil, des interventions sont parfois envisageables comme la pose d’implants, et dans les cas de déformation cornéenne plus modérée du laser cornéen. Sachez toutefois que les améliorations apportées sont inconstantes et inférieures en performances à ce que les lentilles peuvent procurer.
Bonjour docteur, j’ai un keratocone avancé sur l’œil gauche et moins sur l’œil droit. Je porte actuellement des lunettes n’ayant pas supporté les lentilles. Mon objectif est de trouver une solution afin de ne pas porter de lunette ou de lentilles. Y a t il une solution ou une opération qui permet ça? Je souhaite avoir les coordonnées du meilleur spécialiste mondial dans ce domaine svp. Ça ne me gêne pas de faire le trajet et de mettre le prix si j’arrive à trouver une bonne vu sans rien porter.
Il existe déjà un traitement préventif du kératocône; l’arrêt de frottements oculaires intempestifs et appuyés avant que ceux ci n’induisent une déformation permanente de la cornée. Si les pouvoirs publics se saisissaient enfin de ce problème dont je fais l’alerte régulièrement, on pourrait a priori éradiquer ou réduire très considérablement cette affection. Malheureusement, il semble que les consultants qui siègent dans les commissions concernées doutent encore de ce point pour des raisons dogmatiques et par esprit conservateur (le KC est encore considéré par une majorité de spécialistes dont la plupart des universitaires comme une pathologie d’origine primitivement génétique, comme on leur a appris et comme il n’ont jamais voulu douter malgré les évidences logiques et cliniques). L’arrêt des frottements permet de stopper l’évolution de la maladie. Ces préconisations ne sont toutefois pas les bases d’un bon business plan et on a vu récemment aux USA des sociétés venir proposer des tests de dépistage génétique (onéreux) pour les patients désireux de se faire opérer de la myopie. Il n’y a pas de gène pour le KC mais quelques associations ont été décrites (ce qui n’est surprenant car l’épaisseur de la cornée est un trait génétique, et que les patients à cornées fines sont plus à risque de complication post chirurgie réfractive pour la même charge mécanique liée aux frottements). Le kératocône est un enjeu économique; parmi les myriades de chirurgies et de traitements proposés, deux sont suffisants : l’arrêt des frottements et l’adaptation d’une bonne lentille de contact.
La seule contre indication absolue pour les patients atteints de kératocône; se frotter les yeux vigoureusement. L’avion, la plongée sous marine ou le parapente ne sont pas contre indiqués. Si les yeux sont secs ou irrités, ne pas frotter et hydrater ou rincer avec des larmes artificielles.
Bonjour Docteur,
Savez-vous s’il existe des contres indications à prendre l’avion en cas de kératocône (sans port de lentilles)? Mon kératocône a en effet été détecté 4 mois après avoir pris pour la première fois l’avion. Je n’avais jamais eu de problème de vision jusqu’à ce moment là. Ceci est peut être un malheureux hasard mais j’avoue être réticent à l’idée de reprendre l’avion …
Je vous remercie d’avance.
Bonjour Dr Damien Gatinel
cher docteur
pensez vous qu’il y aura un traitement du keratocone dans les prochaines annees?
prendre les compliments alimentaires de vitamines pour les yeux aide il la corenee?
merci
Le CXL ne sert à rien dans ce contexte, malgré la doxa en vigueur (le seul intérêt du CXL est de provoquer l’arrêt des frottements chez les patients qui n’arrivent pas à cesser de le faire avant; la douleur et l’inflammation provoquée, puis la désensibilisation, permettent de réduire les frottements; c’est cher payé pour un geste qui ajoute à une cornée victime d’un stress mécanique répété un stress photochimique). Le CXL n’induit pas de durcissement de la cornée, c’est même plutôt l’inverse. J’ai eu l’occasion d’examiner des patients atteints de KC pour qui un CXL a été effectué d’un côté; l’état biomécanique de la cornée mesuré avec les dernières technologies (ex Corvis ST) est alors moins bon que du côté non opéré! L’idée que le CXL est utile est même naïve sauf pour ceux qui ont un intérêt à le réaliser, ou bien suivent les recommandations « officielles ». Les ingénieurs experts en biomécanique cornéenne à l’origine de la conception de ces machines sont aussi perplexe que moi car ils constatent également que le CXL induit plutôt une variation des indices biomécaniques dans la mauvaise direction. La PKT/PKR seule est préférable (moins de risque d’inflammation) mais les résultats ne sont pas toujours à la hauteur des espérances des patients, il est difficile de régulariser complètement la cornée.
Votre question est pertinente, car l’action des massage quand elle est mal dirigée est susceptible d’enclencher le mécanisme conduisant à la déformation de la cornée et à un « kératocône »; je suis des patients pour qui les massages (trop fréquents et appuyés, qu’ils effectuaient de nombreuses fois par jour) ont entrainé un tableau de kératocône débutant. Il faut presser les paupières « contre elles mêmes » en « pliant » le bord au moment de l’exercice de la pression. L’oeil ne doit pas trop servir de support, car même si vous appuyez sur le blanc (la sclère), la pression intraoculaire est susceptible d’augmenter de manière importante.
Bonjour
Je suis atteinte de blepharite et d’un keratocone. Comment soigner la blepharite avec les soins de paupière sans risquer d’aggraver mon keratocone ? J’utilise des compresses et j’appuie uniquement au niveau du blanc de l’œil, est ce que cela permet de ne pas toucher la cornée ?
Merci beaucoup de votre réponse
Bonjour Docteur,
Mon adaptation aux différentes lentilles étant un échec et voulant une meilleure AV je m’intéresse donc à la PKT.
Plusieurs chirurgiens sont pour la PKT mais en ayant réalisé un CXL avant ou pendant l’opération. Je connais votre positionnement sur le CXL mais je voulais savoir quel était le risque autre que la perte financière de réaliser un CXL en même temps que la PKT.
Mes topographies sont presque identiques durant les 3 dernières années avec une épaisseur de cornée mini de 553microns.
Je vous remercie.
Belle journée
Bonjour Monsieur,
J’aimerais stopper l’évolution de mon keratocone qui je pense est dû en partie à une mauvaise position de sommeil. J’aimerais avoir un masque ou des lunettes à porter la nuit pour éviter des pressions à mes yeux. Connaissez-vous des marques qui font ce type de produit ?
Merci
David
L’arrêt strict des frottements suffit à enrayer la progression du kératocône et éviter les hydrops, qui correspondent aux stades de kératocône très avancés, chez des patients qui frottent de manière très vigoureuse et fréquente. Si vous n’avez jamais eu ce type de complication, il vous suffit de continuer à soustraire vos yeux à tout stress mécanique. Le kératocône n’est pas une affection qui évolue de manière capricieuse ou spontanée comme on le lit dans certains traités (et comme cela est encore considéré par nombre de praticiens pour justifier la réalisation de procédures coûteuses et inutiles comme le cross linking).
Bonjour Docteur,
merci pour vos conseils. Depuis quelques mois je les applique à la lettre. J’ai donc changé ma position de sommeil et arreté de me frotter les yeux. Ma keratocone est plutot avancée, mais avec les lentilles rigides je suis entre 70% et 80% selon la luminosité, parfois plus. Ma cornée est de 370 microns et je n’ai jamais subit d operation sur cet oeil.
Ma question est de savoir comment eviter une erosion de la cornée( corneal hydrops) au fil des années et aussi est ce le fait de ne plus me frotter les yeux m’épargne d’une greffe et de l’érosion. Merci.
Il existe au moins un traitement pour prévenir la survenue du kératocône ; ne pas se frotter trop vigoureusement et fréquemment les yeux. Une fois le kératocône installé, il est trop tard, mais arrêter les frottements suffit pour enrayer la progression. Il ne sert à rien d’essayer de renforcer la cornée, car les traitements actuels échouent à cela, et que même s’ils fonctionnaient partiellement, le durcissement induit serait bien insuffisant pour contrer l’énergie véhiculée par les frottements digitaux. Les cornées nativement « molles » ou fragiles et non frottées ne deviennent pas atteintes de kératocône, elles ont plutôt tendance à s’aplatir progressivement.
Difficile de vous donner un avis sans données objectives; il faut signaler cela à votre contactologue, qui vérifiera les appuis de la lentille, s’il y a des sécrétions, etc.
Bonjour docteur, j’ai un keratocone et suis équipé de lentille sclérale depuis 1 petite semaine. J’ai remarqué sur mon œil gauche (qui est le plus atteint), un voile blanc qui apparaît au bout d’environ 1h de port. Ce voile apparaît 6 fois sur 10.
Avez vous une idée de ce qu’il en est et comment y remédier ?
Merci d’avance pour votre réponse
Bien à vous
Dr Damien Gatinel
cher docteur
pensez vous qu’il y aura un traitement du keratocone dans les prochaines annees?
prendre les compliments alimentaires de vitamines pour les yeux aide il la corenee?
merci
a monsieur Alexandre LANNE
je pense que vous avez une agenosie du sinus frontal essayez de voir un orl
Dans mon expérience large en effectif de patient et temps de suivi, je peux vous assurer qu’il est possible de réaliser une PKR sans crosslinking en cas de déformation cornéenne modérée, à condition de faire cesser la condition qui a provoqué cette légère déformation, c’est à dire les frottements oculaires excessifs. Le dédoublement léger des images en vision de nuit est lié à cette déformation asymétrique légère de la cornée. Le kératocône n’est pas une maladie primitive de la cornée mais la conséquence d’un traumatisme répété. Cette notion va certes à l’encontre de ce qui est enseigné depuis des lustres, mais elle découle d’une analyse logique de cas très bien documentés – notamment les formes unilatérales ou les discordances entre jumeaux monozygotes. Il est à notre qu’à l’inverse, la conception classique mais erronée d’une pathologie spontanément évolutive n’est étayée par aucune donnée tangible: pas de gène spécifique, prédominance de formes sporadiques plutôt que familiales, aucun modèle explicatif pour rendre compte de la déformation, interprétation fausse des cartes topographiques de courbure (les zones « rouges » ne sont pas « en relief » mais simplement plus cambrées, etc etc.) Vous pouvez donc effectuer une PKR seule, ce qui vous évitera un risque inflammatoire et les complications potentielles du CXL dans ce contexte (haze, etc.). Symétriquement, si vous souhaitiez faire évoluer votre kératocône, ce dont je doute, il suffirait de continuer à frotter vos cornées énergiquement avec les phalanges et autres parties dures des mains.
Bonjour Dr.
Je souhaite savoir si la myopie et l’astigmatie dû a un Kératocône LEGER à un oeil peut-être soigné avec une intervention PKR. Au Quebec, les ophtalmologues disent que le Kératocône évolura OU pas même si on ne se frotte pas les yeux. j’ai voulu faire un LASIK qui a été refusé a cause d’un Keratocône leger. Ils disent que même le PKR n’est pas envisageable et me pousse à faire un CXL…ce traitement me fait peur car il semble être accompagné d’une diminution d’acquitté visuelle permanente. Mon métier m’empêche de porter de porter des implants ou des lentilles ou même porter des lunettes. Pour l’instant, je dois forcer légèrement mes yeux pour avoir 20/20 sur les deux yeux. Je souhaite tout faire pour empêcher la maladie d’évoluer et garder une vision parfaite aux deux yeux. Parfois la nuit je vois les sources lumineuse légèrement doublé ( surtout les enseignes lumineuse avec lettre et chiffre)…Si jamais je devais accepter la CXL….puis-je subir un Lasik ou PKR après guérison de la cornée ?
Merci Docteur.
Merci pour votre témoignage, il est effectivement malheureux que l’information sur l’effet causal des frottements sur le kératocône soit si peu diffusée par certain. L’étalement du film lacrymal peut être « perturbé » en cas de kératocône avancé et dans ce cas la prescription de larmes artificielles ou d’agents mouillants locaux peut être indiquée. Il n’y a pas d’inquiétude particulière vis à vis de cela.
Bonjour Docteur,
Tout d’abord, merci pour votre site qui est une mine d’or d’information. J’ai un kératocône aux deux yeux que je pense stabilisé grâce à vos conseils de ne plus se frotter les yeux (et j’insiste bien sur le fait que c’est grâce à vous car JAMAIS mon ophtalmologue ne m’a la suggéré).
J’ai eu mon contrôle annuel il y a une semaine et en examinant mon œil, mon ophtalmologue a parlé de quelque chose qui se produit à cause du kératocône et du fait que les larmes ne se répartissent pas bien, mais je n’ai pas réussi à savoir ce que c’était. Avez-vous connaissance de ce genre de problème? Si oui, est-ce que cela peut-être grave sur le long terme?
Merci beaucoup!
Comme pour tout vaccin, la réponse immunitaire peut être source de réactions croisées, mais ce type de phénomène (rejet de greffe post vaccin) demeure très rare.
Salut Dr j’ai un problème , javais subis une opération de greffe de cornée il ya un an , et j’aimerais savoir votre avis sur l’influence du vaccin coronavirus sur une œil greffe est ce c dangereux de près ou de loin , est ce qu’on peut prendre ce vaccin ou c risqué ,vu la situation de crise vécu actuellement j ss entièrement perdue ,, merci d’avance si vous voulez bien me plairait sur ce point
Bonjour Docteur, je viens dans votre hôpital à Paris Mercredi 10 Novembre. J’ai fait le LASIK en octobre 2018.15 jours plus tard j’ai eu une kératite à l’oeil gauche. Prise en charge et soignée. Quelques semaines plus tard j’ai commencé à avoir des douleurs au dessus de l’oeil droit. J’ai revu plusieurs fois l’ophtalmo qui m’a opéré et ses collègues : on m’a dit il n’y a rien circulé. Je l’ai revu il y a 2 mois et il m’a dit que j’ai une déformation de la cornée mais qu’on ne peut rien y faire.
Insatisfait par cette réponse j’ai vu un ophtalmo d’un autre cabinet ce matin : il pense que j’ai une ectasie post LASIK. Je vais tenter de récupérer mon dossier médical pour voir s’il y avait un kératine avant le laser.
J’aimerai savoir si la prise en charge et le soin de mon oeil gauche peut me donner l’espoir d’enlever mes douleurs à l’oeil droit (qui compense peut être car l’oeil gauche voit double…l. j’espère que vos collègues m’aideront la semaine prochaine je souffre depuis 3 ans et la je fais le déplacement de Strasbourg.
Ce type de nettoyage, si vigoureux, fréquent et appuyé, est tout à fait susceptible d’induire la présence d’une déformation de type kératocône: en voici un exemple réel documenté: https://defeatkeratoconus.com/portfolio-item/case-59/
La conjonction d’une majoration de la presbytie, et peut être d’un vieillissement débutant du cristallin (éblouissemnts). La cornée n’est a priori pas à l’origine des vos troubles, en l’absence de sécheresse oculaire prononcée ou d’opacité significative. Une surveillance est indiquée. Pour le confort visuel, il faut essayer de trouver une correction confortable en lunettes, avec des verres progressifs adaptés, ou bien plusieurs paires de lunettes correctrices (loin vs internmédiaire et près).
Bonjour docteur,
J’ai 49 ans. Depuis juin 2021, je suis face à une problématique visuelle qui ne se solutionne pas.
Mon historique :
Jusque qu’en juin 2021, tout fonctionnait correctement avec le port de lentilles toriques vision de loin (le jour) et des lunettes progressives (le soir).
Mes corrections en lentilles et lunettes étaient les suivantes :
OD (avec amblyopie, 7/10 corrigé) : +0.75 (-1.25) à 170 ° depuis 2012.
OG (10/10 corrigé) : +0.25 (-1.75) à 20 ° depuis 2012.
Avec l’apparition de la presbytie, je travaillais sur ordinateur jusqu’à présent avec mes lentilles et des lunettes de lecture corrigées à +1. J’avais également des lunettes progressives qui fonctionnaient.
Ma problématique
En juin, la vision sur mon œil gauche s’est dégradée et mes corrections lentilles et lunettes n’ont plus fonctionnées. Après consultation de mon ophtalmologue, les nouvelles corrections lunettes ressortent à :
OD (amblyope 7/10 corrigé) : +1 (-1.25) à 170°
OG (10/10 en vision de loin chez l’ophtalmologue) : +0.5 (-2.25) à 20°. Avec l’opticien, j’ai également essayé +0.5 (-2) à 20 °.
Ma problématique est qu’aujourd’hui avec des lunettes vision de loin, des lunettes progressives ou des lentilles souples, je ne trouve aucun confort visuel sur mon œil gauche avec une vision régulièrement floue et/ou déformée. J’ai la sensation de forcer continuellement pour voir. De plus ma vision est fortement dégradée sous les lumières artificielles des magasins et dans la pénombre (ce qui n’était pas le cas avant juin). J’ai également des sensations d’éblouissement avec les phares de voiture. De plus mon œil gauche ne se stabilise plus en vision de loin et de près (ordinateur et lecture de livre). Le travail sur ordinateur même avec des lunettes spéciales ordinateur ne fonctionne pas bien (fatigue et inconfort très rapide). J’ai fait un examen de la cornée ou l’on m’indique un astigmatisme irrégulier OG>OD (S/I vers 1.3) avec épaississement épithéliale inférieur : suspect kératocône. Pachy min 538/537.
Quelles sont les options et traitement possibles pour retrouver un confort et un équilibre visuel d’ensemble que je n’ai plus aujourd’hui et qui me mets en difficulté chaque jour et me pénalise professionnellement. Merci de votre réponse.
Bonjour,
J’aimerais savoir si les frottements induits par l’hygiène palpébrale (notamment le nettoyage réguliers des cils lié à une blépharite chronique) sont de type à être susceptible de provoquer à kératocône ?
Merci d’avance
Si vous avez présenté dans le passé une baisse progressive de la vision avec un astigmatisme évolutif d’un oeil ou les deux il est regrettable effectivement qu’un examen de topographie cornéenne n’ait pas été réalisé plus tôt. En particulier si vous étiez allergique, vous frottiez les yeux et dormiez sur le ventre. A présent il faut cesser tout frottements,. modifier éventuellement la position de sommeil et faire un suivi régulier. Si vous ne vous frottez plus les yeux, alors la déformation de la cornée n’évoluera pas. Il est important de faire très attention car perdre cette habitude n’est pas toujours facile.
Salut docteur
Je ss diagnostiqué keratocone stade 3 après avoir fait la topo pentacam , mais je me trouve perturbée à ce qui correspond la pec , psk d’un côté je me suis choquée comment je ss diagnostiqué tardivement comme ça , malgré je consulte tjrs régulièrement et personne n’a pu découvrir mon keratocone a un stade plus précoce d’où j’ai peur d’une pec aléatoire
J’ai besoin de votre avis à propos mon cas , esk je nécessite un crosslinking ou bien des anneaux ou koi exactement car je fais plus confiance
Il s’agit d’une voie de recherche dont le présupposé est que le kératocône est une pathologie où l’amincissement est « spontané ». Régénérer un tissu dégradé est une piste intéressante pour les kératocônes évolués. Mais le plus intelligent est de prévenir l’apparition ou l’évolution de la maladie. Malgré un faisceau d’évidences qui pointent vers la responsabilité directe, « sine qua non » des frottements oculaires excessifs, il est regrettable que cette pathologie soit encore considérée comme une « fatalité » par nombre de spécialistes « de la vieille école ». Fort heureusement, les ophtalmologistes plus jeunes et sensibilisés à cette conception abordent différemment le kératocône et reconnaissent le caractère inducteur d’un mécanisme traumatique local répété. La prévention du kératocône est possible et devrait être effectuée chez tous les enfants, adolescents et jeunes adultes qui sont à risque de trop se frotter les yeux. Parmi ceux-ci, tous les patients qui dorment sur le ventre avec un appui de la tête prolongé sur l’oreiller impliquant un contact orbitaire.
Bonjour Docteur,
Merci pour ce que vous faites par rapport à cette maladie, vous sauvez des vies.
J’ai une question : que pensez vous des essais de traitement du kératocône par injection de cellules souches ?
C’est Marketing ou vraiment prometteur selon vous ?
Bonne journée
Bonjour Docteur,
Je suis atteint d’un kératocône bilatéral. Je ne me frotte plus du tout les yeux.
Cependant j’ai depuis peu un traitement (blephasol) a utilisé et je dois masser mes paupières Or j’ai peur d’endommager encore + mes cornées. Je masse donc mes paupières sur « le blanc des yeux » sans contact sur la cornée. Est ce que cette technique est valable ou même en massant légèrement sur le blanc cela peut causer un problème sur les cornées ?
Je vous remercie
Merci Docteur Gatinel pour les informations que vous nous apportez.
J’ai 70 ans je suis greffé deux fois des 2 yeux. En 1974 et 1975 à l’Hotel Dieu à Paris puis en 1994-1995 au CHU de Brest pour récidive. J’ai galéré avec des lentilles rigides que je perdais puis avec des verres scléraux ancien modèle. Mais ces interventions et ces appareillages m’ont permis de terminer mes études et de faire une carrière. Effectivement je me frotte les yeux et je dors sur le ventre. mais je n’ai été averti de ces risques par un ophtalmologiste qu’en 1995. on évoquait à l’époque la génétique Effectivement j’ai connu une fratrie de 3 Bretons comme moi tous atteints et greffés. Personne ne m’a proposé un traitement pour limiter mes frottements.
Je pense que ces frottements ont provoqué la récidive qu’on m’avait annoncé improbable à l’époque après mes premières greffes. Sur vos conseils il y a 2 ans je me suis intéressé aux verres scléraux nouveaux et je me suis équipé de verres Spot de chez LAO ce qui me donne une acuité inespérée de 8 à 9 .
Cordialement.
Les masques de protection respiratoires provoquent effectivement de la sécheresse (le flux expiré est dirigé vers le haut, ce qu’il est possible de contrôler en « étanchéifiant » la partie supérieure du masque, avec un micropore adhésif par exemple). Les lentilles sclérales ne sont pas à l’origine d’une progression du kératocône, sauf si pour une raison quelconque ce port provoque un besoin irrépressible de frotter les yeux.
Bonjour, et merci pour votre site très riche en informations.
J’ai été diagnostiqué de keratocone bilatéraux à l’âge de 17 ans il a fortement évolué jusqu’à mes 21 ans, jour où j’ai appris que les frottement occulaire en était la cause.
Mais les dégâts était déjà là, mon œil gauche est fortement atteint (2/10), l’œil droit heuresement esr presque épargné (10/10 avec lunette)
J’ai mainteannt 27 ans, j’ai un contrôle tous les 6 mois pour surveiller l’évolution, et mes deux yeux son stable depuis mes 21 ans, j’ai totalement arrêté les frottements.
J’ai été équipé en lunette pour l’œil droit il y’a 2 ans afin de booster un peu la vue mais l’œil gauche n’est pas corrigé ale par lunette.
Pour en venir à mon questionnement,
À cause des masques j’ai développé une kératite séche au deux yeux, ça devenais Inssuportable, jaindu arrêté de porter le masque mais la sécheresse persistait.
Arès échec de traitment par plusieurs colyre lubrifiant, mon ophtalmologie m’a proposé de tenter lentilles Spot ( laboratoire Lao)
J’ai été équipé il y’a un peu plus de deux semaine au deux yeux, pour le moment la vue est très instables et flou, et cest assez contraignant, en plus elle s’encrassent très vite ( le sérum dans la lentille) .
Mon contactologue ma donner rendez vous dans un ans seulement’
Je m’inquiète de plusieurs chose, est ce que le port de lentille sclerale peux provoquer une aggravation du keratocone ? Est ce que cesr quelque chose sur lequel on a suffisement de recul. Car il est stable depuis presque 5 ans alors je n’aimerai pas tout gacher.
Combien de temps il faut compter pour que la vue se stabilise sur une première adataption ? Car je voyait mieux de l’œil droit avec mes lunettes.
Merci
J’ai déjà observé des cas d’apparition d’astigmatisme au décours d’épisodes de frottements intenses sur une faible durée; le dôme cornéen est effectivement susceptible de subir une légère déformation dont l’origine peut être liée à une désorganisation légère de la matrice des fibres collagènes entrelacées. Dans ce type de situation, l’astigmatisme induit est typiquement de direction « inverse » (aplatissement le long d’une direction verticale ou oblique, et cambrure en regard des méridiens horizontaux).
Bonjour, j’ai eu un orgelet dernièrement et suite à celui-ci (coïncidence ou non) ma vue s’est dégradée avec l’apparition d’une vision légèrement double sur un oeil. Un examen de la vue confirma un léger degré d’astigmatie (déformation inégale) sur cet oeil. Il n’est pas clair pour moi si un frottement excessif durant mon infection aurait pu causer des dommages de type kératocône puisqu’il s’agit d’une courte période. Est-ce qu’un épisode de courte durée mais avec un frottement plus intense pourrait aussi causer des dommages causant une déformation permanente?
Merci beaucoup
Pierre
Il est possible d’engendrer un tableau de kératocône quelle que soit la réfraction initiale. La myopie peut s’accentuer ou apparaître car la déformation cornéenne se caractérise généralement par une augmentation de la cambrure centrale ou paracentrale (concomitante d’un aplatissement périphérique). Cette déformation est provoquée par des frottements appuyés et répétés sur le dôme cornéen. Même si l’augmentation de la myopie est le plus souvent observée (ce qui peut donc être équivalent à une réduction de l’hypermétropie), ce n’est pas toujours le cas. En effet, quand l’amincissement provoqué par les frottements est très inférieur, la « cassure » du galbe cornéen peut induire une cambrure très décentrée vers le bas et un aplatissement central vertical (avec astigmatisme inverse en raison de la cambrure des méridiens horizontaux de la cornée – effet de couple). De ce fait, une réduction de la puissance cornéenne peut être observée (et donc une réduction légère de la myopie, ou au moins une non augmentation de celle-ci). C’est ce que l’on observe par exemple au cours de ce que l’on désigne comme « dégénérescence pellucide marginale de la cornée » (souvent un tableau de kératocône avec déformation épousant les caractéristiques décrites précédemment). Si votre fille ne se frotte pas les yeux de manière excessive, il n’y aura jamais de kératocône.
Bonjour,
Ma fille est hypermétrope et astigmate. Sur sa nouvelle ordonnance de lunettes, son astigmatisme a augmenté. D’après ce que je comprends sur votre site, un des sympt^pmes du keratocone est la myopie, mais est-ce qu’il serait possible d’avoir un kératocone quand on est hypermétrope ?
Il est possible que votre perception soit au moins en partie liée à un biais subjectif (vous faites plus attention aux perturbations visuelles induites par le kératocône). Il est fortement recommandé de ne plus dormir sur le ventre ou côté avec compression prolongée des yeux, car ce facteur mécanique est aggravant et peut entraîner des modifications de la topographie de la cornée (comme en atteste le fait que lorsque les patients arrêtent de dormir comme cela, il apparaît une légère modification du relief cornéen – dans la bonne direction).
Malheureusement, le seul moyen réellement efficace pour le rétablissement d’une vision correcte consiste à adapter une lentille de contact. Cette lentille peut être de type « scléral » (large diamètre, avec appui à l’extérieur de la cornée pour plus de confort). Il faut consulter un contactologue spécialiste pour l’adaptation des cornées atteintes de kératocône.
Bonjour, j’ai le kératocône depuis quelques années et maintenant je sais pourquoi il c’est empiré au fur et à mesure, cela dit j’ai un gros soucis qui m’est apparu y a un an, mon ophtalmo ma préscri des lentilles sauf qu’avec le temps je n’arrivais pas à les supporté, écoulement, démangeaisons, sécheresse, très désagréable, mais aujourd’hui mes lunettes ne me sont plus d’aucune utilité pour l’oeil »affécte » et cela impacte fortement ma conduite, par exemple j’ai du mal la nuit je ne vois quasiment rien, le jour je conduis avec que des dédoublement de la vision, cela commence à me faire peur, que me conseillez vous, je n’arrive pas à supporter les lentilles, les lunettes ne sont pas du grande aide et l’opération comme vous le cité plus haut pas nécessaire ? Que faire?
Bonjour,
Tout d’abord, merci de mettre à la disposition de tous toute cette documentation. En tant que malade, c’est précieux..
J’aimerai vous poser une question, qui relève surement d’une réaction psychologique, mais qui m’inquiète : une fois mon kératocône diagnostiqué, j’ai constaté une baisse de ma vision (vision de loin moins bonne et augmentation des déformations type « ghost images ») lors des 2-3 semaines qui ont suivit. J’ai dû adapter l’ergonomie de mes écrans par exemple.
Il est impossible mes yeux se soient dégradés aussi vite, d’autant plus qu’on m’a tout de suite conseillé d’arrêter les frottements et de changer ma position de sommeil (ce qu’il m’est impossible pour l’instant). Avez-vous déjà eu des cas comme les miens ? Pensez-vous qu’il s’agisse d’une réaction psychosomatique ? Dans ce cas, puis-je espérer une diminution (au moins légère) des symptômes ?
Merci par avance pour votre aide car je ne trouve pas d’information sur internet et mon prochain rendez-vous opthalmo est dans plusieurs mois..
Ces symptômes traduisent plutôt des tractions du vitré, qui est le gel situé en arrière du cristallin et qui occupe la cavité oculaire. Un examen du fond d’oeil est nécessaire. Les frottements oculaires répétés qui sont à l’origine du kératocône peuvent aussi provoquer des lésions vitréo-rétiniennes.
Bonjour,
J’ai un kératocone à l’œil gauche et depuis peu, je constate l’apparition de mouches flottantes et d’éclairs lumineux. Je souhaiterai savoir si les symptômes pourraient être liés au Kératocône ?
Je vous remercie par avance pour votre réponse.
Si votre fille n’est pas allergique et ne se frotte pas les yeux, il peut aussi s’agir d’une évolution liée à une variation de l’accommodation oculaire. La réalisation d’une topographie cornéenne pourrait toutefois être programmée pour éliminer la présence d’une déformation cornéenne pathologique (examen parfaitement non invasif).
Bonjour Docteur,
Ma fille de 7 ans est myope et astigmate depuis qu’elle a 4 ans. Sa myopie est plus ou moins stable, mais au dernier rdv, son astigmatisme était passé de -1,50 à -2.75 (en moins de 6 mois). Je suis très inquiète de cette évolution. Son ophtalmo me dit qu’elle est trop jeune pour avoir un kératocône et que sa cornée est saine (je ne sais pas si elle a fait une topographie). Je ne l’ai jamais vue se frotter les yeux. Dois-je m’inquiéter et consulter un autre ophtalmo ?
Cordialement,
Les déformations infligées par les frottements répétés sur la cornée sont irréversibles, mais on observe souvent, après l’arrêt des frottements, une légère réduction de l’irrégularité de la courbure cornéenne, probablement grâce à un relissage épithélial: le gain n’est malheureusement pas sensible sur le plan visuel car trop modeste.
Merci pour votre réponse. Cela fait sens de dire qu’un Marfan se frottant les yeux pourrait déformer plus facilement la cornée et donc provoquer un kératocône. Je n’ai pas le souvenir de m’être excessivement frotté les yeux par le passé, mais j’ai un terrain allergique (acariens, pollen) + épisodes d’eczéma + temps excessif passé sur l’ordinateur. Il est probable que j’ai modérément frotté mes yeux et qu’un syndrome type Marfan sous-jacent ait accéléré le processus.
Une question se pose alors : si Marfan aplatit la cornée, est-ce que le kératocône de devrait pas s’amoindrir si on arrête les frottements ? Ou alors les déformations sont irréversibles ?
En tout cas je vais aller me faire dépister à Bichat. Effectivement je pourrais simplement être longiligne, d’autant plus que mes mensurations ne sont pas extraordinaires (bien que je sois le plus grand de ma famille), et je suis négatif au test du pouce qui dépasse poing fermé. Les signes squelettiques comme la légère déformation du thorax et le reculement de la mâchoire inférieure (depuis résolu par orthodontie + chirurgie maxillo faciale) laissent tout de même songeur, surtout avec l’association du kératocône. J’ai une forte myopie également, mais il y a pas mal de fortes myopies dans ma famille donc ce n’est pas un signe. J’ai fait il y a un an un examen de l’œil avec pupille dilatée avec un de vos confrères des 15-20, et on ne m’avait rien découvert (pas de subluxation du cristallin), donc je garde espoir…
Votre question est intéressante. Tout d’abord, vous pouvez en cas de doute réaliser un bilan orienté pour un dépistage du syndrome de Marfan (ex: Hopital Bichat); sachez toutefois que l’on peut être longiligne sans en être atteint, mais il est important de vérifier en cas de doutes car ce syndrome peut avoir des conséquences délétères sur le plan vasculaire (anévrysme/ ectasie aortique). Le syndrome de Marfan est intéressant car il permet d’invalider une idée préconçue en matière de kératocône, qui est que ce dernier serait primitivement lié à une anomalie tissulaire (dont le(s) gène(s) impliqués, le mécanisme biomoléculaire seraient encore à élucider), et que les frottements seraient de simples « facteurs de risque », non obligatoire pour l’apparition de l’affection. Le syndrome de Marfan correspond en tous points à une pathologie tissulaire: des gènes sont mutés, responsables de la fabrication d’une protéine appelée fibrilline. Cette anomalie provoque une réduction de la résistance des tissus tels que la paroi des vaisseaux, les ligaments, et les tissus oculaires comme la sclère et… la cornée. La sclère (paroi de l’œil) se distend et s’amincit, et ceci explique l’apparition d’une myopie très fréquente chez le patient atteint de Marfan. La cornée se distend, et s’affine aussi MAIS… elle s’aplatit harmonieusement ce qui est en fait attendu dans le cas d’une atteinte non traumatique, sous l’effet de la pression intraoculaire (l’augmentation du rayon de courbure de la cornée traduit cet aplatissement). Cette observation suffit pour invalider l’idée reçue et communément admise (et qui fait bien les affaires des prescripteurs de cross linking) qu’une altération de la résistance cornéenne, isolée, aboutit à un tableau de KC. En revanche, il est certain qu’en cas de frottement oculaire répété, la cornée d’un patient atteint de syndrome de Marfan se déformera plus rapidement. Ceci explique ce lien classique qui existe dans les vieux traités, et qui peut induire en erreur si l’on n’effectue pas le bon raisonnement… Ayant travaillé dans un centre Marfan il y a quelques années, il est intéressant de constater que certains patients, ) des stades avancés de Marfan (luxation du cristallin, atteinte vasculaire, scoliose marquée, etc) avaient une myopie forte et des cornées tout à fait normales en dehors d’une réduction de la kératométrie (aplatissement, et non hypercambrure centrale ou paracentrale, comme observé dans le KC). Si votre KC est plus évolué du côté droit, c’est que vous frottez plus cet œil, et peut être également avez vous tendance à adopter une position de sommeil qui expose celui-ci à une compression et irritation oculaire nocturne chronique (dormir sur le côté droit ou sur le ventre avec tête tournée vers la gauche).
Bonjour Dr. Gatinel,
J’ai un kératocône moyen oeil droit et début oeil gauche. J’ai 26ans.
J’ai lu sur ce site https://www.keratocone.net/definition.html qu’il y avait une part importante de kératocônes chez les personnes souffrant du syndrome de Marfan.
Je n’avais jamais entendu parler de ce syndrome, mais je me reconnais dans certains symptômes. Je suis grand (1m87), et j’ai toujours été très fin (en ce moment 70kgs mais je faisais plutôt 62-65 il y a quelques années). J’ai de longs doigts fins. J’ai aussi une petite déformation au thorax (un peu projeté vers l’avant côté droit). Jusqu’ici je pensais que tout ceci était normal et délié, aucun médecin ne m’a mentionné le syndrome de Marfan.
Pensez-vous qu’il y ait un lien et que je doive me pencher sur la question ?
La greffe de cornée (lamellaire profonde ou transfixiante) est une intervention dont les indications concernent effectivement les kératocônes très avancés, qui ne sont plus corrigibles en lentilles sclérales ou rigides (présence d’opacités cornéennes stromales prononcées). Les résultats visuels permettent au patient de récupérer une bonne acuité visuelle. La cornée ne se régénère pas seule; le kératocône n’est pas une dégénérescence spontanée de la cornée, mais une affection provoquée et entretenue par des frottements excessifs et répétés, et qui se caractérise par une déformation avec amincissement central.
Bonsoir docteur Gâtinel
Je suis à un stade très avancée de keratocone, je ne supporte plus le port de lentille scelrale depuis 3 ans sur mon œil droit et j envisage la greffe de cornée, cela m à été proposé l année dernière mais j ai peur des risques et si ça va vraiment améliorer ma vue ?
Penser vous qu il existe une façon pour que la cornée se régénère seule ? Est ce qu une fois le kératone installé et la cornée bien abîmé n y a t il pas d autre solutions ? J ai entendu parlé de régénération de cornée avec cellules souches, serais possible avec un keratocone ? Mille fois merci pour le temps que vous prendrais à me répondre
Bonjour Docteur Merci pour votre réponse plus haut!! J’ai vu dans les commentaires que parfois l’usage d’anneaux était préféré au CXL. Je ne sais pas si je dois me tourner vers cela sachant que mon œil droit est vachement avancé au point d’avoir développé un strabisme qui j’ai l’impression est plus marquant qu’avant. On m’avait également dit que la greffe de cornée était requise dans mon cas. Je ne sais pas quelle est la solution.
En tout cas, j’ai cesser les frottements après avoir vu votre énoncé! J’ai même acheter un masque de sommeil afin d’éviter d’avoir un rapport direct avec les yeux lorsque je dors. J’essaie également de dormir sur le dos maintenant. Et je compte prendre rendez-vous avec votre secrétaire.
A priori non, sauf su pour une raison quelconque, l’inflammation sinusale vous aurait fait vous frotter les yeux (ce que l’anesthésie cornéenne, justement, ne favorise pas a priori).
Le cross linking repose sur la notion erronée mais tenace que le kératocône serait une pathologie dont le primum movens est un « ramollissement cornéen » (dont l’origine et les mécanismes intimes demeurent à découvrir ;) ). Comme votre cas le montre, ainsi que ceux des patients atteints de kératocône quand on prend la peine de bien les interroger, le kératocône est une pathologie d’origine mécanique (pas de frottements, pas de kératocône: no rub, no cone !). L’arrêt des frottements est une condition sine qua non pour enrayer l’évolution de la déformation cornéenne. Pour faire simple, l’éviction de tout frottement permettra de stabiliser la déformation cornéenne, CXL ou pas: il n’est donc pas nécessaire de recourir à une technique invasive, qui risque de provoquer une fragilisation accrue de votre cornée. Nous avons pu le vérifier auprès de nos patients bien entendu. Il est aussi recommandé de modifier votre position de sommeil le cas échéant (pas de position sur le ventre ou le côté avec appui sur les yeux – a priori le côté droit si il est le plus atteint chez vous; on observe une forte corrélation entre position de sommeil et côté le plus atteint; ceci souligne au passage le caractère mécanique de l’affection). Vous trouverez toujours de OPH pour vous proposer un CXL, soit par naiveté, soit par intérêt; mais encore une fois cette technique est complètement inadaptée à la prise ne charge du KC ‘son seul intérêt, est parfois d’induire l’arrêt des frottements, en raison de la douleur initiale, puis de la dénervation – réduction de la sensibilité locale par toxicité neurologique). Pour vous donner une idée de la toxicité potentielle du CXL sur une cornée déjà mécaniquement fragilisée, sachez que l’on utilise parfois le CXL pour soigner des infections cornéennes à germes multirésistants (abcès de cornée résistants aux collyres renforcés). Les germes sont effectivement détruits par les UV et le processus oxydatif local, mais il en va de même pour un grand nombre de cellules cornéennes (kératocytes), chargées de la « maintenance » en tissu local.
Bonjour Docteur,
Avant toute chose merci pour ce partage! Depuis que j’ai l’âge de 4ans je suis atteint d’une Conjonctivite allergique permanente ce qui engendrer énormément de frottements au niveaux des yeux. Vers 13ans j’ai senti que ma vue a l’œil droit avait diminué. J’ai donc porté des lunettes. A 20ans on m’a diagnostiqué un Keratocone aux deux yeux avec un œil droit au stade très sévère. ( tout est floue dans cet œil) 1ans plus tard un strabisme a commencer à se développer. Et aujourd’hui je ne sais plus quoi faire, je me demande si le cross linkin sera utile. On m’a dit que parfois il aggravait la vue. Je suis perdu car j’ai mes études de droit d’un côté, je dois lire beaucoup et donc j’ai peur. Que faire ?
Bonjour M. Gatinel,
Vous me suivez pour un kératocône principalement à l’oeil droit.
J’ai appris aujourd’hui que j’avais une déviation de la cloison nasale entrainant une obstruction du côté droit et inflammation des sinus.
En regardant rapidement sur le web, j’ai vu qu’une telle inflammation non traitée peut se compliquer en troubles oculaires, notamment anesthésie cornéenne.
Pourrait-il y avoir un lien entre ça et le kératocône ?
Cordialement,
Amaury
Les fluctuations de correction optique sont habituelles au cours du kératocône, même au sein d’une même séance d’examen ! La répétabilité des mesures est faible en raison de la déformation irrégulière de la cornée; on ne peut donc pas juger qu’un KC progresse si la correction change (un peu comme pour vous) alors que la topographie est stable.
J’ai commis une erreur sur les dates:
0.5 de correction en 2019.
1 de correction mi 2020
Et donc début 2021 une demande d’augmentation de correction de l’astigmatisme
Bonjour Docteur,
J’ai suivi assidûment vos conseils (arrêt total de frottement oculaire ainsi que correction de position de sommeil).
J’ai réalisé 3 topographies sur 1an: résultat topographies identiques aucune évolution des mes keratocones.
J’ai cependant une modification de mon AV et une modification de ma correction d’astigmatisme. En effet je suis passé de 0.5 en 2020 à 1 mi 2021 et à nouveau je constate une baisse de mon AV ma correction demandé une augmentation de correction de mon astigmatisme.
Une modification de correction est elle possible avec des topographies identiques sur le même appareil ?
Je vous remercie
Merci docteur
On fait tout pour qu il n y ait aucun frottements
Cela semble être en bonne voie nuit et jour .
Ils me disent également mieux dormir avec les bras dans le pyjama ..
Les progrès en matière de cornée de synthèse sont rapides, mais rassurez vous, votre enfant n’en aura jamais besoin ;) Une simple prise en charge de bon sens des facteurs de risque de déformation cornéenne garantira son bon pronostic visuel.
Merci pour votre reponse encore une fois très approfondie docteur
Je mise beaucoup d espoir sur le pyjama sans manches qui a été concluant cette nuit en plus des lunettes oculaires (coques +mousses) marque emgidi
Je parlais sur un forum avec d autres personnes
Dans le cas d un enfant de cet âge ,peut on passe directement aux lentilles sclérales ?
Il semble que celles ci soient plus confortables et moins agressives pour la cornée
C est juste une histoire de coût ?
Mon fils dort essentiellement sur le dos et un peu tourné sur le côté ,et cela fait un peu bouger les lunettes
Je. E pense pas que cela soit grave
Nous.ne pouvons pour le moment venir sur Paris (nous habitons la Bretagne ) mais si il s avéré le 2 mars que cela est le kc ,je prendrais rapidement avec vous pour évaluer toutes les possibilités .
Une dernière question je l’espère m apaisera en tant que maman
Quels sont les progrès sur la cornée synthétique en France ?
J ai vu qu en Israël un patient a été opéré avec succès il y a peu .
Encore milles fois merci
Grâce à vous et aux membres de forum j essaye de mettre en place rapidement des choses et j ai foi en la science aussi sur son évolution
Merci pour votre implication
L’évolution ou l’apparition d’un astigmatisme chez un enfant doit faire suspecter un kératocône mais ce diagnostic doit être confirmé par un examen de topographie cornéenne. Ce dernier permet d’évaluer la forme de la cornée et son épaisseur. Il existe un spectre de déformation continu entre les cornées normales et celles où le qualificatif de « kératocône » s’applique de manière indiscutable. Ceci souligne au passage le fait que le KC n’est pas une maladie que l’on a ou que l’on n’a pas, mais l’expression d’un degré de déformation cornéenne variable, fonction du type, de l’intensité et de la durée des frottements oculaires, et aussi de l’ancienneté de ceux ci bien entendu. De nombreuses sessions et articles scientifiques ont été consacrés à l’élaboration de tests diagnostics topographiques ou autres destinés à mieux détecter le KC mais ce problème est en partie biaisé par l’idée que le KC est « présent » ou « absent », et il est toujours difficile de placer un seuil entre le « normal » et l’anormal dans ce contexte (la sémiologie désigne les formes bâtardes difficiles à classer comme « kératocône fruste », « kératocône infraclinique », etc.). Concernant votre fils, le degré d’astigmatisme encore modéré laisse augurer d’une faible déformation, mais la réalisation d’un examen de topographie cornéenne (Orsbcan, Pentacam, ou équivalent) est indiquée. Si vous avez l’occasion de venir sur Paris elle pourra être réalisée plus tôt que début mars si vous êtes particulièrement inquiets. Sur le plan thérapeutique, le traitement du KC est celui de sa cause: les frottements intempestifs. Les frottements oculaires nocturnes sont difficiles à contrôler au début et l’idée de ne pas enfiler les manches du pyjama est astucieuse. Des coques oculaires de protection peuvent être associées. La position de sommeil ventrale doit être évitée. Si les frottements intempestifs et vigoureux cessent, il n’y aura pas de déformation cornéenne. Le paradoxe dans l’approche classique du KC est de considérer que la cornée peut se déformer « seule » (sous le simple différentiel entre la pression intraoculaire et la pression atmosphérique), alors qu’aucun modèle ne permet d’expliquer cela sans l’adjonction d’une force externe responsable d’un amincissement et d’une fragilisation focale (locale). De nombreux praticiens sont plus intéressés de profiter de l’angoisse de parents ou de patients pour leur proposer des chirurgies comme le CXL qui sont destinées selon eux à stopper la maladie; ceci prouve qu’ils ne comprennent pas (ou ne veulent pas comprendre) la nature de cette affection. Ceci peut s’expliquer par une inertie intellectuelle, un conformisme de pensée, ou des intérêts moins nobles; admettre l’évidence, que le KC est avant tout une pathologie mécanique et comportementale oblige à réviser une approche potentiellement lucrative pour une enquête minutieuse et la prescription de simples recommandations de bon sens…
Bonjour docteur
Je reviens vers vous suite à mon message concernant mon enfant de 10 ans suspicion de keratocone
Je suis très anxieuse à ce sujet
J ai observer depuis plusieurs jours les nuits de mon fils
En journée il ne frotte pas ses yeux (ou plus car je ne sais pas il le faisait à l’école et ça semble être passé inaperçu ) mais il frottait la nuit avec le bas des paumes de la main
Nous avons je pense trouver le moyen de stopper les frottements via les lunettes de nuit et un pyjama ou il n enfile pas les bras .
Je lis que si apparition avant la puberté ,les risques d évolution sont très forte notamment si apparition brutale (ce qui semble le cas avec l astigmatisme de mon fils passée de 0,25 à -1,50 et de 0 à -1,25
J ai peur qu il perde rapidement sa vue
J ai parcouru toutes vos réponses et je vois donc que il ne Faut pas faire le cxl
Mais vous parlez de pkr ,cela consiste en quoi ? Cela se fait sur un enfant si jeune ?
Je dois m’attendre à ce que mon fils soit greffe dans quelques années vu son astigmatisme actuel et une évolution rapide ?
Quels sont vos retours avec des enfants de cet âge que vous avez reçu et accompagnés ?
La topographie n est que le 2 mars
J ai fortement insisté pour que l’on Ophtalmo l avance ,car il ne souhaitait la faire que dans six mois .
Sur un forum de discutions un papa disait que son fils avait perdu 80 % de sa vue en six mois
Il a eu le kc à 10 ans et demi
Dans le pire des cas à quoi dois je m attendre ?
Les hormones avec la puberté accroient l aggravation ?
Nous pensons si le kc est détecté ,venir vers vous pour un suivi
Je suis désemparée ,je lui ai réduis la lecture alors qu il adore ça et va lire toute la journée
Merci docteur
Dans un premier temps, le plus important est de cesser tout type de frottement oculaire appuyé, et remédier aux éventuelles causes de ces frottements.
Ensuite, tout dépend du degré de KC, c’est à dire du degré de fragilité et de déformation de vos cornées. En cas de déformation modérée (« kératocône fruste »), il est parfois possible de réaliser une intervention de type PKR.
Bonjour
Je suis allée dans une clinique consulter un spécialiste des yeux pour envisager une opération pour ne plus porter de lunettes.
Suite aux examens,le spécialiste m’a découvert un keratocone bilatérale.
Grande déception pour moi.
J’ai bien compris l’importance de ne plus se frotter les yeux.
Pouvez me dire si un jour je pourrais bénéficier d’une opération pour améliorer ma vue sans lunettes.
Cordialement
Le frottement oculaire excessif est la cause du kératocône, et participe à son évolution quand il persiste. Il est donc beaucoup plus important de rassembler vos efforts pour mettre un terme à ces frottements, plutôt que de recourir à des techniques de chirurgie invasives, peu efficaces comme le CXL (si ce n’est par le biais d’un arrêt des frottements en post opératoire, lié à l’inflammation initiale puis la dénervation tardive, en raison de la toxicité de la procédure sur le tissu cornéen et les cellules qui participent à son renouvellement). La société Emgidi commercialise de nombreux types de masques de protection oculaire, et vous trouverez facilement leur site internet pour commander un de leurs masques. Il est recommandé de modifier votre position de sommeil afin d’éviter d’appuyer sur vos yeux la nuit.
Bonjour docteur, je découvre votre site, merci pour ce partage. Ayant un keratocone bilatérale, avec très forte astigmatie mais bien corrigé, je souhaite acquérir des coques de protection.
En effet je me frotte les yeux et je comprends l’importance et souhaite mettre toutes les chances de mon côté. Mon ophtalmologiste me conseille le cross linking suite à l’évolution de ces deux dernières années. Je ne veux pas passer par cette option. Pouvez vous indiquer un modèle de coque de protection pour la nuit ? J’ai cherché et ne trouve pas, pouvez vous décrire plus précisément ?
Merci encore
Merci beaucoup pour votre réponse docteur
Le travail prolongé sur écran, en particulier sur des horaires étendus vers le soir est un facteur de risque pour la survenue de frottements oculaires répétés et excessifs. Il est heureux que vous ayez réalisé qu’il était important de cesser définitivement ces frottements, ce qui vous mettra à l’abri de la progression de la déformation cornéenne (qui définit le kératocône), en soustrayant le dôme cornéen aux stress mécaniques répétés. Le véritable traitement du kératocône débutant correspond en fait à l’éviction des frottements et la prise en charge des causes de frottements (allergie, sécheresse, tics, position de sommeil ventrale ou de côté, etc.). Dans votre cas, il est convient de vérifier que la position de votre écran soit la plus ergonomique possible (écran situé légèrement sous la ligne du regard). Il est conseillé de faire des pauses régulières, en regardant au travers d’une fenêtre toutes les 20 minutes par exemple pour reposer le regard. Les collyres sont nécessaires, bien que vous ayez bien compris qu’ils ne sont pas toujours efficaces pour calmer l’irritation. Certains collyres sont plus « visqueux » et permettent une protection plus efficace. La prise en charge d’une blépharite associée est souvent nécessaire. Un bilan allergologique est indiqué si vous avez des antécédents d’allergie. Pensez aussi au contrôle de l’air ambiant à votre domicile: s’il est trop sec (chauffage éléctrique), essayez de l’humidifier, et aérez régulièrement.
Le kératocône est défini par la présence d’une déformation cornéenne qui provoque des aberrations optiques comme l’astigmatisme, la myopie, que l’on peut corriger en lunettes, mais également d’un contingent d’aberrations optiques dites de « haut degré » (le terme plus simple d’astigmatisme « irrégulier » recoupe cette notion) que l’on ne peut pas corriger en lunettes. De plus, ces aberrations interfèrent avec la correction de l’astigmatisme, c’est à dire qu’en fonction de divers paramètres comme le diamètre de la pupille, la cible observée, la correction permettant d’obtenir la « meilleure vision » peut fluctuer. L’astigmatisme engendré par le kératocône peut atteindre des valeurs assez importantes, et ceci est également un problème en correction lunettes (déformation de champ vers les bords du verre). Pour résumer, la correction en lunettes d’un « kératocône » n’est pas unique. Les lentilles rigides, qui « moulent » la face antérieure de la cornée, permettent de corriger l’astigmatisme régulier et irrégulier, et ce type de correction doit être privilégié pour la correction du kératocône.
Bonjour docteur, je voudrais savoir si le fais d’avoir un keratocone, agis sur la correction de vue? Pour ma part cela fais quatre fois que je change en l’espace de deux mois, la correction de vue de ma paire de lunettes.A chaque fois au bout d’une heure je commence a avoir des picotements ainsi que des maux de tête.
Cordialement
merci beaucoup docteur
Bonjour docteur ,
J’ai un kératocône de stade 1 à l’oeil droit et un léger amincissement de la cornée au niveau de l’oeil gauche diagnostic après topographie cornéennes , je les développé durant la confinement en passant plusieurs heures devant mon ordinateur cela m’a provoquer une sécheresse oculaire et j’ai commencé à me frotter excessivement les yeux , ma question est es qu’il a d’autres remède contre la sécheresse oculaire autre que le collyre car étant étudiant je passe l’intégralité de mon temps devant un ordinateur est cella me cause des douleur à la tête sachant que je porte des lunettes anti lumière bleue et corrections de loin pour l’oeil droit
Il est difficile de répondre à vos interrogations sans examens. Il faudrait éliminer une rotation postopératoire de l’implant torique dans un premier temps, je pense que votre chirurgien a du procéder à cette vérification. La capsulotomie n’est pas dangereuse, même si elle expose à certaines complications (augmentation du risque de décollement de rétine chez les myopes). Toutefois, quand une capsulotomie est nécessaire, elle est la seule technique à même de traiter la cataracte secondaire, et doit être généralement réalisée.
La topographie cornéenne est rarement présente dans les cabinets d’ophtalmologie de ville, plutôt en milieu spécialisé (service hospitalier, centre pratiquant la chirurgie réfractive). Ce point est regrettable dans le contexte du dépistage du kératocône (repérer tôt les patients qui se frottent beaucoup les yeux et leur expliquer l’intérêt d’arrêter pour enrayer la déformation). Le kératocône ajoute généralement de l’astigmatisme myopique à la myopie préexistante. Le kératocône est la première cause d’apparition et d’évolution de l’astigmatisme. La cataracte peut également produire une variation de l’astigmatisme, mais le contexte clinique est différent. Le kératocône est avant tout une pathologie d’origine mécanique: déformation cornéenne et amincissement provoqués par des frottements oculaires excessifs et répétés dans le temps. Dès qu’une déformation du dôme est suffisamment prononcée, un astigmatisme apparaît. Les astigmatismes en question sont typiquement inverses ou obliques; il sont liés à un aplatissement vertical (la « cassure », c’est à dire la zone de cambrure accentuée est généralement située en inférieur, car c’est là que les frottements s’exercent en général) avec courbure accentuée en latéral; cette augmentation provient du fait que lorsqu’une structure se déforme, il existe certaines contraintes topologiques qui conduisent à maintenir constante la courbure moyenne de la cornée (dit un peu trivialement; toute cambrure accentuée est compensée par une cambrure diminuée à un autre endroit)
bonjour docteur
merci pour votre réponse très rapide et pour la clarté de vos explications
j ai quelques questions a vous poser
1/ Comment peut on savoir si le médecin réalise une topographie cornéenne?
2/ quels sont les conséquences du kératocone si présent avec une si forte myopie ?
3/ l astigmatisme peut il évoluer sans kératocône?
Encore merci docteur gatinel
philippe
Bonjour Docteur
J’ai été opérée de la cataracte des deux yeux en juillet dernier. J’ai un keratocone à l’oeil gauche
OD vision de près satisfaisante. c’est ce que je souhaitais pour pouvoir me passer de lunettes au quotidien
OG (implant torique) vision de loin miraculeuse après l’opération mais qui s’est dégradée dans les jours qui ont suivi . Maintenant je n’y vois avec cet oeil ni de près, ni de loin avec mes nouvelles lunettes prescrites pour la vision de loin.
Je suis retournée voir mon ophtalmologue qui a diagnostiqué une cataracte secondaire et m’a fait sur le champ une intervention au laser yag.
Aucune amélioration et je suis très réticente a faire la deuxième séance de laser prévue.
Mes questions :
– est il possible que le port de ma lentille rigide ait faussé la prise de mesure sur la cornée le matin de l’opération et en ce cas l’implant peut il être repositionné sans risque ?
– une capsulotomie présente t elle un danger ? le mieux étant l’ennemi du bien
Merci infiniment de votre réponse .
On ne peut exclure la possibilité d’un kératocône, en particulier si votre fils se frotte beaucoup les yeux – le kératocône n’apparaît ni n’évolue spontanément, contrairement à ce qui est écrit ailleurs, de manière illogique d’ailleurs puisque l’on ne voit pas bien comment une telle désorganisation tissulaire pourrait survenir sans l’impact d’un facteur biomécanique (tous les mécanismes biochimiques ou biocellulaires jusqu’ici inovqués sans confirmation ne peuvent pas expliquer l’apparition du tableau typique de kératocône). Répétons que devant toute modification de l’astigmatisme avec myopie chez un enfant ou un adolescent, il est nécessaire de faire pratiquer un examen de topographie cornéenne. Si celle-ci révèle un début d’amincissement avec déformation, il faut alors réaliser une enquête approfondie sur les frottements oculaires et leurs causes (allergies, sécheresse, fatigue avec travail ou jeux sur écran le soir tard, etc etc). Une fois les frottements identifiés, il faut tout mettre en oeuvre pour les faire cesser (ce qui inclut parfois la nécessité de revoir la position de sommeil). Ceci permet de stabiliser la déformation et d’éviter de recourir à des interventions comme le CXL (dont l’effet n’est pas réellement démontré, au delà d’un effet collatéral bénéfique qui est que les patients ne frottent généralement plus l’oeil opéré en raison de la douleur puis de l’inflammation locale générée, et ensuite « grâce » à une désensibilisation liée à l’atteinte neurologique locale).
bonsoir et bonne année
dans le cadre d’un patient jeune prenons par exemple mon fils qui avait un astigmatisme de -2.25 OD en qui est passé à 3.75 en decembre 2020 . il possède également une forte myopie de -7 et de -9?
est il possible que ce soit un keratocone ?
bonne journée et encore joyeuse année 2021
Le plus important est de comprendre que le kératocône n’est pas, contrairement à ce que l’on lit encore un peu partout, une pathologie héréditaire, mais le résultat d’un traumatisme cornéen répété (les frottements oculaires). C’est pour cela qu’il est parfois difficile de poser le diagnostic de kératocône devant des déformations cornéennes mineures (désignées par le terme de « kératocône fruste »). Il est crucial que votre fille cesse de frotter ces yeux, ce qui implique un bilan étiologique destiné à identifier la ou les causes de frottements, et celles-ci incluent souvent l’allergie et l’atopie chez les jeunes. De même, il existe des formes de « kératocône » induites par une position de sommeil inappropriée (sur le ventre ou le côté, avec appui prolongé de l’oeil sur l’oreiller, le bras, etc.). Vous pouvez venir me consulter à la Fondation Rothschild ou l’un de mes assistants spécialisés dans la prise en charge moderne, éthique, et non invasive du kératocône. Votre fille échappera à la réalisation de techniques inutiles comme le cross linking, erronée de principe puisqu’il ne sert à rien de durcir la cornée (le durcissement n’est même pas quantifiable in vivo!), alors qu’il est très important de ne plus traumatiser mécaniquement la cornée. Le port de coques de protection nocturne est souvent indiqué. L’arrêt des frottement permet logiquement de stabiliser la déformation de la cornée; on observe souvent d’ailleurs une petite amélioration après l’arrêt des frottements et de la possible compression nocturne chronique.
Bonjour,
Je voulais vous remercier de votre retour et des explications fournies avec autant de clarté et de transparence. Votre démarche me semble relativement rare au sein de la profession.
Cependant, ma fille n’ayant pas encore reçu de diagnostic établi de keratocone par l’ophalmologiste (libéral et reconnu) qui la suit, j’hésite à engager directement une démarche alternative. Peut-être devrais-je attendre 6 mois et la réalisation d’un nouveau test pour aviser en fonction du « verdict ». Cependant, j’aimerai d’ores et déjà vous demander votre contact pour pouvoir fixer une consultation avec vous si jamais le KC est confirmé. Faites-vous partie du centre de compétence KC à la Fondation Rothschild?
En vous en remerciant
Bien cordialement
Ingénieur Tunisien Age 37 ans je souffre d’un kératocône fruste stable et c’est confirme depuis les topographie cornéenne pendant des années
j’ai essayé avec les lentille souple et rigide , mes yeux sont un peu sensible
j’ai consulté plusieurs spécialiste référents en Tunisie, un seul très renommé en tunisie m’a dit que je suis opérable sans risque ( insiste bien sans risque) , sans me donner les détails technique de l’opération.
les autres par unanimité m’on dit que c’est risqué malgré que le kératocône est fruste (stable) , peut être TRAN PKR mais c’est toujours un peu risqué ( évolutions des année après )
une TRANS PKR sans contact bien évidement est il toujours pas rassurante pour mon cas
je suis tes articles et tes publications depuis des années ainsi connu en Tunisie comme une référence dans ce domaine Monsieur , je voudrais avoir ton avis stp
Voilà mon dernier orbscan :
OS
SIM Ks
Astig -1.5 @ 11°
Maximum 44,5 D @ 101°
Minimum 43.0 D @ 11°
3 mm Zone
Irre +/- 1.2 D°
Mean power 43.8 +/- 0.9 D°
Astig power 2.0 +/- 0.9 D°
5 mm Zone
Irre +/- 1.3 D°
Mean power 43.8 +/- 0.9 D°
Astig power 2.6 +/- 0.9 D°
thinnest point 529 Um @(0.4/0.3)
kappa 3.47° @38.38
Best fit values
Astig D/° +2.57/+1.02
OD
SIM Ks
Astig -2.6 @ 10°
Maximum 44,6 D @ 100°
Minimum 42.0 D @ 10°
3 mm Zone
Irre +/- 1.5 D
Mean power 43.4 +/- 1.2 D
Astig power 3.6 +/- 1.0 D
5 mm Zone
Irre +/- 1.5 D
Mean power 43.4 +/- 1.1 D
Astig power 3.9 +/- 1.1 D
thinnest point 543 Um @(0.5/1.0)
kappa 5.11° @175.16
Best fit values
Astig D/° +4.04/+95
je voulais comprendre est ce que je dois oublier l’opération à jamais et revoir les lentilles s’il ya des nouveautés
Dans mon expérience, l’arrêt des frottements suffit pour stabiliser la déformation cornéenne. Le manque de clarté de diagnostic en matière de KC est surtout lié au manque de clarté dans l’esprit de ceux qui continuent à considérer cette affection comme d’origine primitivement génétique (aucun gène identifié, et des cas de discordances entre jumeaux monozygotes, etc etc..). Le kératocône est la conséquence directe des frottements répétés et excessifs; on observe tous les stades intermédiaires entre cornée régulière (non ou peu frottée) et cornée très déformée (très très très frottée), et il est donc difficile de tracer une ligne déparatagant les malades des sains, alors que l’enjeu est ici de neutraliser le ou les gestes responsables. On note souvent, quand les frottements cessent et que la position de sommeil est modifiée (passage à une position sur le dos sans compression nocturne prolongée) une légère amélioration en matière de topographie cornéenne. Le crosslinking n’a qu’une vertu (mais fait courir des risques de complications, enviroin 15% des cas; retards de cicatrisation, haze, infections, etc.): les patients arrêtent de frotter en raison de l’inflammation générée dans les suites opératoires. Si ce que je vous avançais était erroné j’aurais de graves soucis avec les parents d’adolescents à qui j’ai expliqué ceci alors qu’ils étaient déjà munis d’une indication de CXL émanant d’un autre confrère… Pour l’anedcote, l’un des parents d’un de mes jeunes patient travaille à l’HAS!! Et ne regrette pas de m’avoir confié son fils qui va très bien depuis qu’il a cessé de frotté (il avait lui même reçu une prescription de CXL). Les patients qui ont cessé de frotter, dormi avec des coques oculaires de protection, n’ont pas progressé. Considérer le KC comme une pathologie qui est susceptible d’évoluer spontanément sert les intérêts de ceux qui promeuvent le CXL (cross linking). Nous sommes, dans le service que je dirige, à l’origine de la théorie « no rub, no cone », qui est récente (auparavant les frottements étaient considérés comme de simples « facteurs de risque », un peu comme si on considérait que le brossage des dents trop énergique était un « facteur de risque » de gingivopathie!). Cette proposition est récente (quelques années) mais elle a fait ses preuves et est dorénavant considérée comme très crédible, à tel point qu’un article récent publié dans une revue scientifique de référence par une équipe américaine conduite par un des pionniers de l’exploration cornéenne et du kératocône (Rabinowitz) conclut qu’elle est certainement validée pour de nombreux cas, mais qu’il existe, peut être, aussi des formes de KC « spontanées » (conception classique d’une pathologie d’origine primitivement dégénérative)… même si cela n’est certain selon Rabinowitz, qui a consacré plusieurs décennies à tenter d’isoler un ou des gènes spécifiques à la maladie (en vain). C’est tout son mérite que de remettre en cause ses propre conceptions et d’étudier avec soin une hypothèse alternative. Cela dit, il est souvent très difficile de cesser les frottements, même si l’on peut, en s’attaquant à leur cause (allergie, sécheresse, fatigue visuelle, position de sommeil, etc.) souvent en réduire le besoin. Je peux recevoir votre fille en consultation à votre convenance pour évaluer son cas. Notre protocole est simple: enquête sur les frottements, détermination de leurs causes, explications, et premier contrôle à un mois, puis 3 mois, puis 6 mois, puis un an avec comparaison objective des cartes de topographie et d’épaisseur cornéenne. Si les recommandations sont suivies, une stabilisation voire une légère amélioration est observée. Il est par ailleurs intéressant de constater que les patients qui progressent sont ceux qui n’arrivent pas à cesser les frottements, et ceci valide au passage le bien-fondé de la conjecture « no rub, no cone ».
Bonjour,
Ma fille de 18 ans a du réaliser en novembre dernier des tests pour la détection d’un kératocone. Myope depuis ses 11 ans, elle a développé depuis qq années un astigmatisme qui augmente.
Suite à ces tests (orbscan, aberrométrie…), le diagnostic n’a pas pu être posé clairement par le médecin qui évoque malgré tout des suspicions. Elle doit repasser des tests de cornée d’ici à 6 mois, un an. Je me demandais combien de temps fallait-il attendre pour poser de manière fiable un diagnostic de keratocone (6 mois ou 1 an entre 2 tests?)
Si le diagnostic s’avère positif, j’ai lu sur une étude de l’HAS que chez les jeunes patients, le Cross linking est la première étape à réaliser pour stabiliser la maladie(avant les anneaux intracornééens) car le risque d’évolution est probable qd la maladie se déclare jeune .Est-ce une méthodologie que vous validez?
Sinon, vous mettez en avant le fait que d’arrêter de se gratter les yeux permet de stopper l’évolution du Keratocone mais comment ne pas se gratter les yeux. Il me semble que c’est un geste incontrôlable ? Et ensuite sur des jeunes patients, la maladie une fois diagnostiquée pourrait-elle être endiguée uniquement par l’arrêt de ces gestes ou faut-il opter pour des traitements chirurgicaux?
Enfin, quelles sont les meilleures équipes pour suivre un keratocone à Paris?
Merci de vos précisions.
Votre question n’a rien de bête. Mais le recul sur le minoxidil semble aujoud’hui suffisant (cette molécule est ancienne – anti hypertenseur vasodilatateur utilisé dans cette indication capillaire depuis au moins 30 ans; initialement, les patients sous minoxidil oral signalaient une augmentation de leur pilosité! L’indication comme anti chute capillaire est ainsi née de cet « effet indésirable »). Concernant le kératocône, on sait aujourd’hui, au moins dans mon département, une chose: la déformation cornéenne et sa progression dépendent des frottements oculaires. Les stopper (ainsi que toute manoeuvre mécanique intempestive répétée) est suffisant pour contrôler l’évolution de la déformation. A moins que l’utilisation du minoxidil en lotion ne déclenche chez vous de féroces envies de frotter vos yeux, vous ne risquez donc rien.
Bonjour Docteur,
Tout d’abord merci pour ce site web qui est très enrichissant et rassurant. J’ai été diagnostiqué d’un KC à l’oeil gauche l’année dernière, et depuis je ne touche plus mes yeux par peur d’aggraver la déformation. Ma question est peut être bête, mais j’ai commencé à appliquer de la minoxidil sur mon cuir chevelu pour stopper la chute de mes cheveux, et j’ai lu dans les effets secondaires que cela pouvait provoquer des troubles de la vision. J’aimerai savoir si la minoxidil peut aggraver un KC? Je sais que nous n’avons pas assez de recul ni sur le KC ni sur la minoxidil, mais je demande quand même.
Merci d’avance
Tout d’abord, il faut confirmer l’évolution par la réalisation de cartes différentielles et une bonne interprétations de celles-ci; ces cartes doivent être obtenues avec la même machine pour être comparées. De fausses impressions de progression peuvent être liées par des variations instrumentales, surtout en cas de kératocône. J’ai vu des cas où l’arrêt des frottements et la modification de la position de sommeil provoquait une variation de la topographie cornéenne (régularisation légère) qui avait pu être confondue avec une progression. La progression se caractérise par un amincissement cornéen et une augmentation significative de la cambrure cornéenne en regard des zones déjà les plus cambrées. Visuellement, la myopie et/ou l’astigmatisme progressent. La répétabilité des examens topographiques est moindre en cas de kératocône et il convient de répéter éventuellement la topographie en cas de doute.
Bonjour Docteur,
j’ai arrêté les frottements oculaires et modifier ma position de sommeil et pourtant mon kératocone continue d’évoluer.
Savez-vous quels autres effets mécaniques peuvent participer à la déformation de la cornée.
Merci pour votre aide.
Il est effectivement possible que l’inflammation provoquée par le cross linking ait provoqué une certaine instabilité au niveau de la surface cornéenne, notamment de l’épithélium. L’inflammation peut aussi contribuer à accentuer l’amincissement du stroma cornéen. Au delà d’un certain stade (généralement très avancé), la cornée peut devenir plus instable biomécaniquement, particulièrement si elle est fortement amincie. Les fluctuations sont particulièrement marquées entre le réveil et plus tard dans la journée. Le recours à la greffe de cornée (greffe lamellaire profonde) peut être parfois une solution pour retrouver une vision utile, si le port de lentille rigides ou sclérales est impossible.
Il est parfois difficile de retirer les lentilles étant donné leur diamètre important. Il peut être tenté de trouver une technique alternative pour pour la retirer en la faisant glisser ou basculer sur le côté par exemple.
Bonjour, suite à un diagnostique de KC, je porte une lentille rigide sclérale sur l’oeil droit depuis 3 ans. J’éprouve beaucoup de difficultés à la retirer le soir. Je pratique bien les méthodes qui m’ont été préconisées pour la pose et dépose de la lentille. Je met la ventouse sur le bord inférieur pour appliquer un effet de levier mais malgré cela, j’ai beaucoup de mal à décoller la lentille qui fait elle-même un effet ventouse sur l’oeil. Mon oeil est vraiment tiré vers l’avant et à force de tirer, la lentille fini par se « décoller ». Ceci est vraiment désagréable.
A force de tirer comme cela est-ce que je ne risque pas de déformer encore plus la cornée?
Est-ce que ce problème est régulièrement rencontré par d’autres patients et plutôt normal, ou est-ce que je ferais mieux de m’en inquiéter?
Merci pour vos conseils.
Cordiales salutations
Bonjour Docteur,
Tout d’abord merci pour le partage de vos connaissances et de votre expérience qui sont d’un grand soutien.
J’ai 28 ans et je suis atteint d’un kératocône bilatéral détecté il y a 4 ans. J’ai subi un CXL sur les deux yeux, et notamment sur l’œil droit qui ne présentait pourtant pas d’évolution. Suite à l’opération j’ai constaté sur cet œil une vision trouble et on m’a prescrit un collyre anti inflammatoire qui a fonctionné.
Depuis 2 ans l’oeil droit évolue avec un astigmatisme de plus en plus prononcé, et ce malgré l’arrêt complet des frottements et une position de sommeil surveillée. Je suis extrêmement rigoureux vis à vis de cela notamment suite à la lecture de vos travaux et de vos réponses.
De ce fait, je me désemparé et impuissant face à cette maladie qui évolue malgré mes efforts pour la stopper ou du moins la ralentir.
Cependant mon acuité visuelle varie énormément sur l’oeil droit, de façon totalement aléatoire et il m’arrive même parfois de retrouver une vision ne nécessitant pas de correction (au moins de près), même si c’est très épisodique et de plus en plus rare.
Est ce normal pour un patient atteint de Kératocone d’avoir une variation d’AV ? Est ce que le CXL a pu avoir un effet néfaste sur la cornée (film lacrymale, épithélium, membrane de Bowman…) et accentuer l’astigmatisme ? Quels examens supplémentaires je peux réaliser ? Vos confrères que j’ai consulté n’ont pas pu m’apporter de réponses convaincantes.
Désormais, la plupart du temps j’ai un astigmatisme très prononcé de près et de loin (avec une sensation de gêne), mais les épisodes avec une AV améliorée me laisse l’espoir qu’il s’agit d’ autre chose que le Keratocone, surtout que je ne me frotte plus du tout les yeux.
En espérant que vous puissiez me répondre,
Vincent
Un léger pincement, même répété de manière quotidienne, n’est pas à l’origine du kératocône, qui découle de lésions traumatiques plus soutenues et répétées. Si votre KC a été découvert vers la soixantaine, c’est que la déformation est modérée, et que les frottements que vous avez effectués étaient moins violents et intenses que chez un patient pour lequel la découverte intervient plus tôt dans l’existence.
Bonjour Docteur,
J’ai 71 ans et on m’a détecté un kératocone il y a une dizaine d’années sans m’en expliquer l’origine que je viens de découvrir en lisant avec intérêt votre explication sur ses causes mécaniques toutefois je n’ai pas souvenir d’avoir eu cette mauvaise habitude de me frotter les yeux par contre comme je porte des lentilles souples depuis 40 ans j’ai tous les soirs effectué un léger pincement de chaque oeil pour retirer chaque lentille et la mettre à tremper pour la nuit. Au bout de 40 ans j’ai donc ainsi pincé chaque oeil environ 15000 fois est ce que ce ne serait pas là la cause de l’apparition de mon kératocone ?
Avec mes remerciements et mes meilleures salutations
L’accouchement n’a pas d’influence sur le kératocône, ce qui importe est de ne pas frotter ses yeux ou les soumettre à un stress mécanique quel qu’il soit. L’accouchement n’en est pas un pour les yeux.
Bonjour docteur étant diagnostiqué avec un kératocône depuis maintenant plus de 10ans et ayant subit deux crossliniking sur mes deux yeux gauche et droite qui sont au stade 1 et deux je mets des lentilles sclerales aussi et pour le moment ma maladie est stable et_il vrai que pour un accouchement une césarienne est préférable a un accouchement naturel pour mon cas et Merci
L’utilisation d’anneaux intra cornéen permet en effet de réduire une partie de la déformation cornéenne. L’effet des anneaux est toutefois partiellement imprédictible, et s’ils réduisent une partie de l’astigmatisme ils n’ont pas ou peu d’effet sur la myopie moyenne de l’oeil. Idéalement, ils s’adressent aux patients qui ont un astigmatisme peu prononcés. Sinon il faut prévoir une photokératectomie réfractive associée dans un deuxième temps (PKR). Ces techniques ne sont pas sources d’un arrêt de l’évolution en elles-mêmes. C’est bien l’arrêt des frottements qui est (logiquement puisqu’il en est la cause) le facteur permettant de stopper l’évolution du kératocône. Prétendre durcir la cornée avec le CXL n’est pas raisonnable, puisqu’in vivo on n’observe aucun durcissement significatif, et que cette approche est comparable à celle d’un dentiste qui proposerait à un patient qui se frotte mal les dents de durcir ses gencives. IL est bien entendu préférable d’opter pour de bons gestes, et dans le cas du kératocône, la « sanctuarisation » des globes oculaires est primordiale. Bien évidemment certains intérêts convergent pour proposer toujours plus de gestes et d’interventions. Sachez par ailleurs que contrairement à la chirurgie réfractive, où il existe une obligation implicite de résultat, la chirurgie du kératocône profite d’une certaine « tolérance » à l’échec; on blâmera la maladie en cas de résultat imparfait. Ceci permet d’appuyer certaines indications opératoires parfois hasardeuses, et il est vrai que la vision est tellement entravée par les KC évolués, qu’une dégradation supplémentaire n’est pas forcément un facteur repoussant pour la chirurgie. ON remarque qu’à l’inverse, les chirurgiens un peu « agressifs » répugnent fortement à opérer en CXL l’oeil le moins atteint quand celui-ci est pourvoyeur d’une vision correcte. Si cette technique était sûre et efficace, dans leur logique, il conviendrait d’opérer cet oeil pour prévenir l’apparition/l’évolution de la maladie. Rappelons pour conclure, que le meilleur outil correcteur pour la réhabilitation visuelle du kératocône est l’adaptation d’une lentille rigide: il est par ailleurs peu invasif, mais évidement moins « spectaculaire » qu’une intervention (ou une série de), pourtant bien inférieure en matière de qualité de correction. Dans certains cas de KC peu évolués, quand les frottements ont cessé, et que la déformation cornéenne est ainsi stable, signalons qu’il est souvent possible de réaliser une PKR seule, topoguidée ou non (la somme des chiffres de myopie et d’astigmatisme doit idéalement être égale à moins de 5 D pour un effet optimal). Les résultats sont cependant souvent un peu moins bons que pour les yeux myopes et astigmates indemnes de kératocône.
Bonjour Docteur,
J’ai été diagnostiqué d’un Kératocône donc je m’informe sur la maladie. J’ai vu récemment une présentation montrant des résultats assez impressionnants en utilisant anneaux intra cornéens qui permettraient d’améliorer la topographie cornéenne en optimisant leur placement puis laser Topoguidé pour lisser les irrégularités. D’une part la topographie cornéenne est quasi normalisée et d’autre part un effet réfractif sur la myopie et l’astigmatisme régulier est possible.
Qu’en pensez-vous ?
Par contre je pense comme vous qu’on surestime l’utilité du CXL pour entraver l’évolution du Kératocône. La combinaison laser topoguidé et arrêt strict des frottements serait-il la clef pour être soigné de cette maladie ? L’inconvénient que je vois est que le laser peut augmenter la sécheresse des yeux donc il faudra redoubler de vigilance sur les frottements.
J’espère avoir l’opportunité de me faire suivre par un grand spécialiste comme vous pour vaincre le Kératocône. Bonne journée à vous.
La chirurgie est souvent proposée de manière un peu abusive pour le kératocône car malheureusement, les résultats des interventions sont moins efficaces que l’adaptation de lentilles rigides. Cette adaptation devrait être la première méthode de correction à proposer chez les patients atteints de kératocône avéré. Et bien entendu, il est crucial que vous ayez cessé de vous frotter les yeux.
Bonjour j’ai 39 ans j ai su que je suis atteinte de keratocone à l âge de 31 ans auparavant j ai porté des lunettes et je sens toujours que j ai des troubles de vision mon ophtalmo m’ a conseillé des séances de correction ça n a pas amélioré. En 2011 j ai visité un autre ophtalmo qui a diagnostiqué la keratocone mais il ne m a pas bien expliqué la situation et il m a proposé une intervention chirurgicale les anneaux au debut j’ai accepté mais par la suite mon opticien m’ a proposé de visiter un autre ophtalmo bien connu en Tunisie il m a bien expliqué ma situation (keratocone très avancé ) il a refusé les interventions chirurgicales et il m a proposé les lentilles rigides depuis 2012 je porte ces lentilles mais l inconvénient ce que je ne supporte pas la poussière la vapeur la lumière j ai toujours les larmes et dès que je les enlève je commence à frotter
Est ce qu il ya une autre solution ou d autre lentilles permanentes
Merci
A priori le kératocône n’est pour rien dans cette aspect: il faudrait consulter un spécialiste en pathologie orbito palpébrale; parfois, une chute de la paupière peut donner à l’oeil un aspect « plus petit ».
Bonjour,
Atteinte d’un keratocone j’ai lu avec plaisir vos articles et j’ai surtout bien compris cette pathologie.
Je suis récemment suivie à la fondation Rotshild malgré que mon keratocone a été diagnostiqué il y’a plusieurs années.
J’ai un œil plus petit que l’autre je pense que la lentille rigide y a beaucoup contribué.
Je focalise dessus, jusqu’à ne plus sortir.
Y’a til un moyen de remédier à ça ?
Merci.
Bonjour docteur oui effectivement je ne me frotte plus les yeux sur conseil de mon ophtalmo c’est pour cela qu’il m’a dit qu’il fallait impérativement ne plus frotter les yeux pour stopper l’évolution du kératocône.merci pour votre réponse et vos conseils.
La première chose à faire quand on pose le diagnostic de kératocône est de réaliser un interrogatoire détaillé pour mettre en évidence la réalisation des frottements oculaires et en déterminer les facteurs de risque pour mieux les traiter (allergie, position de sommeil sur le ventre ou le côté, sécheresse oculaire, etc.). Il ne faut plus du tout frotter vos yeux afin d’enrayer l’évolution de la déformation cornéenne. Le kératocône est en effet l’expression d’une déformation et d’un amincissement de la cornée consécutifs à ces frottements excessifs. Les conséquences visuelles sont fonction du stade du KC, plus accentué du côté plus frotté (le gauche chez vous, essayez de vérifier si vous ne dormez pas en appui sur la tête du côté gauche).Au départ, la déformation provoque typiquement l’apparition d’un astigmatisme myopique que l’on peut corriger en lunettes. On découvre d’ailleurs parfois un (ou deux) kératocône(s) débutants chez les patients qui consultent pour une chirurgie réfractive lors de la réalisation systématique de la topographie cornéenne. Quand les frottements persistent et sont particulièrement vigoureux et répétés, la déformation devient telle qu’elle induit une forme d’astigmatisme plus sévère que l’on ne peut plus ou plus totalement corriger en lunettes. Dans ces situations, les patients signalent typiquement la perception d’images fantômes; la lune apparaît dédoublée voire démultipliée dans le ciel nocturne. C’est à ce stade qu’il est nécessaire de tenter une adaptation en lentilles rigides ou semi rigides. Votre oeil droit est à un stade où l’on peut encore corriger en lunettes, mais l’oeil gauche est déjà malheureusement trop atteint pour que la correction en lunettes soit efficace. Je vous conseille de consulter un spécialiste en lentilles de contact pour kératocône (contactologue) pour améliorer votre vision.
Bonjour docteur merci de prendre quelques minutes Afin de m’éclaircir sur mon l’état actuel de mes yeux j’ai 32 ans il y a un ans je voulais changer de verre de vue car je voyais de plus en plus mal de mon œil gauche après une visite chez un ophtamologue il a pas pu diagnostiquer donc il m’a conseillé de faire une topographie cornéenne et après la réalisation de la topographie on m’a diagnostiqué un keratocone stade 3 pour l’œil gauche et sade 2 et demi pour l’œil droit.
Sans vraiment m’orienter il m’a juste demandé de voir un optométriste pour mettre des lentilles rigides mais l’oprometriste ma conseillé de commencer avec le changement de verre de vue donc je suis passé a – 1,50 et le résultat l’œil droit je vois bcp mieux mais tjr l’œil gauche floue et qui me fait depuis en plus mal depuis 15 jours.
je m’adresse a vous docteur avec une grande inquiétude car je vis une dépression énorme… que faire svp merci.
Cette chirurgie est théoriquement possible dans votre cas, car même si le kératocône n’évolue plus, il ne sera jamais possible d’effectuer un LASIK. Il est important que vous ne vous frottiez plus les yeux, mais si le KC est stable, c’est que c’est déjà le cas.
Bonjour docteur, voilà mon soucis je suis myope-8 OG et-9 OD le laser et pas réalisable car ont ma diagnostiqué un keratocone il y a 2 ans. Mon dernier rdv du moi de mars chez l’ophtalmo m’a dit que ma vu n’avait pas bouger et que mon keratocone n’avait pas évolué donc je voulais savoir si c’était possible de me faire opérer avec des implants oculaire ? Merci.
La première question à vous poser est celle de l’efficacité visuelle de cet anneau. Le but premier et unique d’un anneau intra-cornéen est d’améliorer la vision de l’oeil atteint de kératocône. Ceci peut être difficile à apprécier sans lunettes, mais en principe, la pose de l’anneau doit réduire l’astigmatisme et donc simplifier la réalisation d’un équipement optique type verre de lunettes. En revanche, la pose d’un anneau rend souvent plus difficile le port d’une lentille. Par ailleurs, l’anneau de stabilise pas le kératocône ni ne soigne cette maladie. Seul l’arrêt des frottements oculaire peut le permettre. Si votre correction n’est pas ou peu améliorée par l’anneau, il est préférable de le retirer. Sinon le repositionner. Il existe malheureusement un certain abus dans l’indication des anneaux intra-cornéens. Leur efficacité n’est pas contestable dans certains cas, mais ceux-ci ne sont pas si fréquents; et par ailleurs, la vision n’est jamais aussi améliorée que par la pose d’une lentille rigide (ou verre scléral pour les kératocônes très évolués) en cas de kératocône.
A priori, il est possible d’instiller ce collyre avant de porter vos verres scléraux. Vous pouvez essayer de diluer le produit dans le sérum physiologique en espérant qu’il n’y ait pas de turbidité particulière résultant d’un mélange imparfait entre le collyre et le sérum.
Bonjour docteur,
J’ai un kératocône bi-latérale depuis 30 ans avec une greffe de cornée sur un oeil en 1998.
je suis équipé de lentilles mini sclérales qui me corrigent parfaitement.
j’ai de la kératite sèche mon ophtalmo m’a donné des collyres lubrifiants à mettre le soir après le retrait des lentilles. Afin d’améliorer l’efficacité, puis-je mettre une goutte de Théalose dans mes lentilles (en complément du sérum phy) avant la pose le matin ?
Merci d’avance
Salut Docteur Gatinel, merci beaucoup pour votre site.
J’ai 26 ans, j’ai un kératocône bilatéral troisième stade, je me suis fait une pose d’anneaux intra cornéens sur mon œil gauche ya 18 jours de celà des le premier jour j’ai ressenti que quelques choses me pique la paupière quand je cille mais je l’ai ignoré les premiers jours, je me suis dit que c’est peut être dû a l’incision sur la cornée mais cette désagréable sensation est toujours présente j’ai le sentiment que l’extrémité de l’anneau me pique la paupière j’ai pas encore passé mon contrôle Vu le coronavirus vu le confinement et les couvre-feu j’ai pas pû me déplacer chez lui
j’ai fait une consultation chez un autre médecin qui ma dit que l’anneau est mal placé il faut un réajustement de l’anneau je me demande si c’est possible et normal ??
Et si ca va se régler normalement ?
Ou bien il faut le retirer complètement je m’inquiète vraiment prière de m’aider votre avis va m’orienter et me rassurer docteur, je vous prie de répondre quand vous verrez mon commentaire
Merci
Cordialement ?
Merci de votre témoignage qui pourra également rassurer d’autres patients: le kératocône n’est PAS une maladie qui évolue spontanément, avec une greffe de cornée comme menace planante, mais l’expression somme toute conforme aux lois de la physique d’une déformation physique devenue permanente (plastique) de la cornée sous contrainte (les frottements oculaires répétés). Il serait bien entendu aussi présomptueux que dangereux de vous affirmer que l’arrêt des frottements va permettre de stabiliser la déformation (même si cela semble tout à fait logique) sans en avoir vérifié le bien-fondé: vous pourrez vérifier en consultant le site http://www.defeatkeratoconus.com que les patients qui observent ces préconisations (arrêt des frottements, modification de la position de sommeil) n’ont pas d’évolution. A l’inverse, ceux qui avouent continuer à se frotter (c’est souvent bien difficile d’arrêter brutalement) continuent de progresser. Il faut parfois redouter l’existence de frottements inconscients pendant la nuit; aussi je vous conseille de porter une ou des coques de protection oculaire la nuit (au moins au début) ou bien un masque de protection mousse des yeux (voire ici éventuellement: http://www.emgidi.com). Les facteurs qui engendrent une irritation oculaire, un prurit, doivent être traités pour réduire le risque de continuer à se frotter les yeux. Malheureusement, ce discours est plutôt rare en dehors de mon unité à la Fondation Rothschild. Le « mythe » d’une dystrophie cornéenne d’évolution imprévisible à la peau dure, notamment chez les plus vieux praticiens et sert aussi parfois à justifier la réalisation de gestes chirurgicaux inutiles comme le cross linking. Pour savoir si la déformation évolue, il faut toujours réaliser une carte différentielle (deux examens consécutifs dans le temps sur le même topographe cornéen). Sur le site http://www.defeatkeratoconus.com vous trouverez de nombreuses informations et exemples d’évolution favorable après arrêt des frottements. La cornée ne reprend pas une forme « normale », mais l’arrêt des frottements (et la levée de la compression nocturne éventuelle) permettent à l’épithélium cornéen de relisser un peu le galbe de la cornée. Ces modifications sont au moins du même ordre que celles provoquées par la réaction cicatricielle au CXL (nous pensons d’ailleurs que les légers changements topographiques après CXL sont liés à cette réaction et l’arrêt des frottements en post opératoire). N’hésitez pas à partager votre expérience et ressenti sur les réseaux sociaux où des groupes de patients atteints de kératocône partagent des informations (pas toujours justes malheureusement…)
Bonjour Docteur Gatinel, merci beaucoup pour votre site et votre article.
J’ai 32 ans, j’ai été chez mon ophtalmo ce matin, qui a trouvé bizarre que mon astigmatie ait beaucoup augmenté depuis 18 mois. Il m’a dit qu’il était était possible que j’ai un kératocône. Cela m’a fait un choc, je ne savais pas ce qu’était cette maladie et que l’on envisage toujours le pire dans ces cas (une maladie qui conduit à la cécité…). J’ai passé tout le reste de la journée à glaner des infos sur Internet en me tourmentant par rapport à ça, car même si en fin de compte l’on ne risque pas la cécité, cela à l’air quand même bien embêtant.
Ce soir, au fil de mes recherches sur cette maladie je trouve votre article et votre site, qui m’apaise beaucoup car vous donnez une explication qui me parait avoir du sens, qui est conforme avec mon expérience personnelle et qui en plus aboutit à fournir un levier d’action très concret et pratique. C’est beaucoup moins déprimant de savoir qu’il existe un moyen d’agir pro-activement pour stopper l’évolution, plutôt que de se dire « peut-être que cela va dégénérer jusqu’à devoir greffer une nouvelle cornée » sans savoir pourquoi.
Dans mon cas, j’ai été très négligeant avec mes yeux, car cela fait plus de deux ans que je n’ai plus de lunettes, mais que je porte seulement des lentilles (je suis myope). Par conséquent, je portais mes lentilles du matin au soir, et tous les jours. Cela avait finit par me donner des démangeaisons aux yeux, et j’avais conscience de me frotter souvent les yeux. Dès demain, je vais aller me racheter des lunettes.
Vous écrivez que la déformation peut être élastique/réversible au début. Comment savoir si l’on est au stade où l’élasticité demeure, ou bien si la déformation est permanente ?
Lé répétabiité des mesures topgoraphiques, même réalisées avec le même instrument n’est pas absolue, et il est possible qu’il s’agisse d’une fluctuation de mesure. La kératométrie de l’oeil gauche a légèrement diminué, ce qui incite à penser qu’il n’y a pas de progression réelle de votre déformation cornéenne. Si vous avez cessé de frotter vos yeux, aucune évolution n’est à redouter. Le plus intéressant pour apprécier les changements est de réaliser des cartes différentielles, qui apportent plus d’informations et de manière plus globale.
Bonjour
Excuser moi vous ne m’avez pas répondu à mon message qui date du premier janvier 2020,quej’attend depuis.
Merci.
Merci pour votre témoignage. Certains (de très rares) patients atteints de KC me signalent, sur internet, ne pas s’être frotté les yeux. Dans mon expérience directe avec les patients que j’ai examiné directement, TOUS ceux qui présentent un KC s’étaient, parfois transitoirement au cours de leur existence, excessivement frotté les yeux. Mais certains n’avaient pas conscience de cela jusqu’à ce que des explications détaillées soient prodiguées. Parfois, les patients effectuent des gestes de friction, appui, qu’ils ne considèrent pas être des frottements, ou bien frottent le matin au réveil dans un état semi conscient. Par ailleurs, il existe bien de rares formes où un nombre important de membre d’une même famille présentent la maladie. Dans la littérature médicale, les formes de ce type (« familiales ») ne représentent que 10% des formes de KC, car dans 90% des cas, il s’agit au contraire de formes dites sporadiques (qui surviennent d’ailleurs chez le patient qui est le seul à beaucoup se frotter les yeux, dans les fratries où seul un membre est atteint). Il ne faut pas confondre cause et susceptibilité génétique. Dans les familles ou la cornée est génétiquement plus fine, et où existent des facteurs de risque pour les frottements (allergie), alors il n’est pas du tout anormal que s’observent plus qu’un cas isolé de kératocône. Un raisonnement par l’absurde permet de contredire la possibilité d’une atteinte « spontanée », car en dehors d’un mécanisme d’action local, on ne peut engendrer une déformation cornéenne sans l’application de contraintes mécaniques répétées. Les pathologies bien documentées sur le plan génétique et qui provoquent une altération du collagène cornéen n’entraînent pas un tableau similaire à celui du kératocône. Le kératocône est une affection qui est souvent découverte quand le patient se plaint de baisse de vision, cette baisse traduit la présence d’une déformation cornéenne déjà significative, où l’on retrouve systématiquement une réduction d’ épaisseur limitée au centre de la cornée. Bien souvent, la position de sommeil est orientée vers un appui sur l’oeil atteint (ou le plus atteint), ce qui renforce encore la présomption d’une atteinte mécanique locale: dormir sur le ventre est un facteur de risque pour le kératocône. L’amincissement provoqué par la répétition du stress mécanique conduit à une défaillance biomécanique locale, et la déformation qui accompagne celle-ci. Les formes unilatérales de la maladie sont toutes liées à des frottements unilatéraux, et bien souvent, des frottements sur l’oeil qui est « comprimé » la nuit sur l’oreiller. Si votre lentille est moins adaptée, il faut réaliser une topographie cornéenne pour vérifier que la déformation n’a pas progressé, et essayer d’étudier les causes qui pourraient entraîner une irritation locale. La durée de vie des lentilles hybrides est limitée, et il faut également envisager un renouvellement de celles-ci.
Il est effectivement déconseillé d’utiliser de l’eau du robinet pour nettoyer les lentilles ou leur étui. Dans le cas de l’adaptation des lentilles rigides sur les yeux atteints de kératocône, les sensations d’inconfort local sont fréquentes, en raison de la déformation du dôme cornéen qui entraîne des zones d’appui et de frottement particulières. Il faut éventuellement trouver une géométrie plus adaptée pour cette lentille afin de vérifier si cela pourrait avoir un impact positif sur votre sensation de confort oculaire.
La ménopause ne devrait pas provoquer de modification structurelle de votre cornée. En revanche, si la sécheresse oculaire augmente, alors vous pourriez avoir envie de vous frotter les yeux de manière réactionnelle et ceci pourrait alors provoquer une évolution du kératocône.
Bonjour Docteur,
On m’a découvert un kératocône bilatéral à 44 ans et je suis asthmatique et allergique, j’ai arrêté de frotter mes yeux et je mets des collyres antihistaminiques et j’ai changé ma position de sommeil mon kc n’a pas évolué mais maintenant j’ai 46 ans et je suis une femme et j’approche à grand pas de la ménopause et je me demande si avec la ménopause mon kc ne va pas évoluer car on sait ce que les hormones peuvent agir sur la vue et les dents et j’en ai vu les conséquences sur mes dents et ma vue lors de mes 3 grossesses . Qu’en pensez vous ?
Cordialement
Bonjour,
Je voudrais vous remercier dans un premier temps d’avoir pris le temps de répondre à l’ensemble des messages qui m’ont beaucoup aidé. J’ai été diagnostiqué d’un kératocône il y a maintenant 2 mois. J’ai 23 ans. Je suis au stade 2 sur les deux yeux. Grâce à vos précédents messages très encourageants, j’ai très fortement réduit les frottements voir presque arrêter. J’ai beaucoup d’allergie et conjonctivite, de ce fait lorsque j’étais plus petit j’ai commencé à me frotter les yeux, et cela sur le long terme jusqu’au jour où on m’a indiqué que j’avais la maladie. Je me suis comme beaucoup de monde renseigné sur internet et je suis tombé sur votre site avec toutes ces réponses motivantes et intéressantes. Aujourd’hui, je porte des lentilles rigides depuis 1 mois et quelques jours qui m’ont permis d’augmenter ma vision : 12/10 aux deux yeux. Au départ mes lentilles droite et gauche tombées fréquemment et ce déplacé très facilement sur mes yeux. Aujourd’hui, je n’ai plus ce problème ou du moins que très peu. Mon adaptation sur ma lentille gauche se passe plutôt bien. Sur ma lentille droite, j’ai au bout de quelques heures des dépôts qui brouillent complètement ma vue. J’ai l’impression d’avoir un voile blanc devant ma lentille. Je la retire alors pour la nettoyer et cela redevient normal. Mais au bout d’une heure, ce problème revient… Je ne sais pas quoi faire. C’est parfois compliqué… J’utilise la solution d’entretien precilens B5 chaque jour et procare pour déproteiniser mes lentilles une fois par semaine. Pensez-vous que sont les produits qui ne me conviennent pas ? Il est possible que ce soit des résidus de ma conjonctivite qui se loge derrière ma lentille. Je ne sais pas quoi faire… Je vois même mieux sans ma lentille droite après une heure de port… Mon optométricien m’a dit que je pouvais nettoyer l’étui à lentilles avec de l’eau. Mais je ne sais pas quoi faire, car, je lis beaucoup sur internet qu’il fallait éviter de faire cela pour cause de contamination par des amibes. Qu’en pensez-vous ? Il m’arrive lorsque je pose mes lentilles que ça me pique l’œil durant quelques secondes, trouvez-vous cela normal ?
Encore merci,
Cordialement,
Nicolas
Bonjour,
Je me permets de réagir face à votre insistance concernant le fait que le kératocône soit dû aux frottements et absolument pas à la génétique.
J’ai un kératocône bilatérale depuis l’adolescence (aujourd’hui au stade 4), mes trois frères et sœurs sont également touchés. Ma mère a été diagnostiquée à la ménopause.
Concernant les frottements, je ne me suis JAMAIS frotté les yeux, et j’insiste bien sur le JAMAIS. Mes frères et sœurs idem.
Je pense personnellement que cette maladie est multifactorielle, et que certains cas peuvent être dus aux frottements, mais d’autres cas sont certainement génétiques ou épigénétiques.
Sinon depuis peu, je ne peux plus porter ma lentille hybride gauche. Elle me cause une kératite systématiquement même après 2 semaines sans lentille + collyres + pommade pour soigner la kératite.
Il faut savoir que j’ai 31 ans, mon kératocône est stable depuis 9 ans environ.
J’ai pris rdv avec ma contactologue, mais ce n’est pas avant un mois, et je m’inquiète beaucoup.
Est-ce possible que cela soit juste la géométrie du cône qui a évolué sans toutefois s’être aggravé, et qu’il faille juste établir une nouvelle correction ? Ou bien, pensez vous que c’est plus grave?
J’espère que vous pourrez me rassurer…
Merci.
Bonsoir
Excuser moi ,Je rectifie la date de la première topographie est 29.08.2017
La deuxième est 31.12.2019
Merci.
Bonne année et meilleurs vœux
Voilà je viens de faire ma deuxième topographie cornéenne ,la première étant faite le 29.08.2019
J’ai relevé quelques indications essentielles:
Œil droit au 29.08.2019
K1 :45 Dpt ,K2:49,3Dpt ,K-Max 47 Dpt
,Astg :4,3 Dpt , Pachymetrie:538 microns
Le 31.12.2019 œil droit
K1:44,9 Dpt,K2:49,3Dpt K-Max 47,0Dpt
Astg:4,5 Dpt, pachymetrie:534
Œil gauche au 29.08.2019
K1 :43,6 Dpt,K2:45,3Dpt ,K-Max :44,4Dpt
Astg:1,7Dpt ,Pachymetrie 584 microns
Le 31.12.2019 Œil gauche
K1:43,0 Dpt ,K2:45,0Dpt ,K-Max :44,0Dpt
Astg:2,1Dpt ,Pachymetrie : 567 microns
Âge 19 ans ,aucune intervention chirurgicale je porte dès lunettes ,ma question je me frotte plus les yeux et ce depuis pratiquement deux Annnés comment ça se fait que j’ai perdue plusieurs microns à ma corné gauche sachant que c’est le même appareil topographieque.
Qu’en pensez vous de cette évolution. Merci beaucoup de votre attention.
A vos questions je réalise que vous n’avez pas lu en détail les pages de ce site consacrées au kératocone et au cross linking. Cette technique de CXL ne sert à rien dans le cadre d’une maladie provoquée par les frottements oculaires répétés, qu’il suffit d’arrêter! La déformation n’evoluera plus, ce qui logique, puisque la déformation fait suite aux frottements, comme le coup de soleil fait suite a l’exposition aux UV. Le kératocone n’est pas, comme enseigné dans des traités classiques et dorénavant poussiéreux, une dystrophie évolutive d’origine génétique et de mécanisme biomoléculaires inconnus, mais, comme en attestent les travaux entrepris dans mon unité, le raisonnement logique et l’observation, qui devraient être les piliers de la médecine fondée sur les preuves, une déformation cornéenne avec amincissement d’origine primitivement mécanique. Du moins jusqu’à preuve du contraire, ce qui n’est pas près d’arriver… Au contraire, le flux incessant de patients fraîchement diagnostiqués conforte cette position, que rejettent certes les dogmatiques et ceux pour qui prescrire des interventions coûteuses à de patients inquiets et désorientés représente une confortable opportunité d’exercice sans grand risque. Ne frottez plus, même devant les écrans, et tout ira bien. Continuez de frotter et la déformation évoluera, avec ou sans cross linking…
Merci pour votre témoignage. Le cross linking n’a pas d’intérêt (pour vous) et si vous cessez de vous frotter les yeux alors la déformation ne progressera pas. Les frottements répétés provoquent au fil du temps un affaiblissement de la cornée: elle de déforme, et c’est quand cette déformation est suffisamment avancée que les premiers symptômes visuels apparaissent : en moyenne deux ou trois ans après le début des frottements incessants (allergie, irritation, ou parfois fatigue avec mauvaise position de sommeil). Le kératocone est plus marqué (la cornée plus amincie et déformée au centre) du côté ou vous frottez plus (ce qui est logique), qui est aussi celui sur lequel vous dormez très probablement. Tous nos patients, des qu’ils arrêtent de frotter, deviennent stables, sans besoin de CXL. Par ailleurs, ceux qui continuent de frotter évoluent, même après le CXL! Celui ci n’est pas une réponse logique au KC, et est de plus inefficace vis a vis de son objectif qui est de durcir les cornée (le durcissement n’est pas observé chez les patients et quand bien même il surviendrait il serait insuffisant vis à vis de la force des doigts quand on frotte. Les greffes n’arrivent qu’aux patients qui, pour des raisons psychologiques, ou parce que l’on ne les a pas bien informé, se sont tellement frotté les yeux pendant de nombreuses années, que la déformation cornéenne est majeure. Évitez les interventions chirurgicales souvent inutiles et décevantes, et traitez la cause des frottements. Plus de conseils sur le site http://www.defeatkeratoconus.com
Bonjour Docteur , j’ai un kereatocone dans les deux yeux .stade 3 (j’ai fait un cross llinknig) oil droit et satde 2 oil gauche.
m’a question est ce qu’il faut faire le cross linking dans le 2eme oil sachant mon ophta m’as dit qu’il faut attendre un autre 6 mois.
2eme Question : je suis développeuse Informatique (toute la journée devant l’écran), est ce que ce travail va aggraver mon keratocone (la ou j’arrive plus a me concentrer sur mon travail )
Merci.
Bonjour Docteur et merci pour ce site bon tout d’abord j ai 23 ans et je suis diagnostiqué du keratocone fruste oeil gauche et stade 2 oeil droit .c’est vrai que j’avais toujours l’habitude de frotter mes yeux et surtt oeil droite , le docteur m’a demandé de faire un cross linking pour les 2 yeux , et une lentille rigide pour oeil droite .mais franchement docteur je crois que je vais utiliser que les lunettes et je vais faire un cross linking j’ai arreté de frotter mes yeux et maintenant j’essaie de régler ma position de dormir c’est difficile ar ce que par fois je trouve que je frotte mes yeux pendant que je suis dormis .docteur svp est ce que je peux arretter la progression de cette maladie sans utiliser une lentille ? et quel est lepourcentage d’etre obliger de faire un gref de corné dans le future ?
En cas de kératocône modéré et stable, ce qui revient à ne plus se frotter du toutes yeux, la PKR est possible, a condition que le degré de myopie et d’astigmatisme soit compatible avec ce que peut corriger cette technique. Il n’y a pas besoin d’y ajouter un cross linking, car encore une fois, l’arrêt des frottements oculaires suffit pour enrayer la progression du kératocône…
je souffre d’un kératocone depuis l’age de 30 ans debut stade 2 , d’aprés les topographies sur 3 ans il est stable
j’ai utilisé des lentille souple et régide pour améliorer la vue par rapport les lunette mais malheureusement j’étais trés sensible à ces lentilles (larmes et picottement)
J’ai visité trois chirurgien connu en tunisie pour la possibilité de faire une opération lazer corrective , meilleur technique sans risque et complication
le premier trés répandu en tunisie m’a dit que c’est faisable votre cornée et épaisse , ton kératocone est stable , on peut chosir la meilleur technique sans risque
les deux autres connu aussi m’ont dit que c’est trés risqué lasik ou pkr meme avec peu de risque (opération douleureuse)
je suis un peu perdu , moi j’ai suivi des articles qui parlent des technique avancés comme le countour vision ( basé sur l’empreinte yeux) qui est une technique trés optimale en traitement lazer
le premier docteur m’a donner aucun explication sur la technique que va le procéder et insiste toujours qu il n’y a pas de risque
tu peux m’aider stp et me clarifier un peu la différence total des avis aprés consultation
Remarque : premeir docteur m’a fait plsueirs topographie et meme avancé
Ce type d’indication est parfaitement abusive. Si votre vision est convenable en lentilles, il ne faut surtout pas essayer de réaliser une chirurgie de type cross linking ou pose d’anneaux. Le kératocône est une maladie de la cornée dont nous avons identifié la cause première: les frottements oculaires. C’est pour cela que le kératocône est souvent retrouvé chez les patients allergiques (qui se frottent les yeux qui démangent), et parfois chez les patients qui dorment sur le ventre ou le côté en appuyant sur les yeux (l’irritation provoquée semble être également à l’origine de frottements). Le kératocône est une déformation cornéenne qui est causée par les frottements répétés, et dès que l’on arrête les frottements, il n’y a plus d’évolution. De fait, le cross linking n’a pas d’intérêt si l’on arrête de se frotter les yeux. La stabilisation du kératocône après CXL est d’ailleurs très certainement liée à l’arrêt des frottements; nous avons observé les mêmes effets après cessation des frottements (la cornée n’est pas durcie, comme dans le CXL qui échoue à cela, mais elle tend à s’applatir légèrement une fois les contraintes liées au frottements levées). https://defeatkeratoconus.com/results-of-our-online-study/ et https://defeatkeratoconus.com/cross-linking-like-effect-cessation-of-eye-rubbing/
Votre question n’est pas idiote, car toute affection oculaire chronique la fait naître en général dans l’esprit de celui qui en est atteint. Encore une fois, répétons que le kératocône n’est pas une maladie spontanément évolutive contrairement à ce que l’on peut lire ou infuser dans l’esprit des patients (parfois pour leur faire accepter la réalisation « en urgence » d’une intervention type cross linking ou pose d’anneau). Le kératocône est une affection dont la cause primitive est mécanique: frottements répétés et vigoureux. Arrêter défitivement ces frottements c’est arrêter l’évolution du kératocône: https://defeatkeratoconus.com/results-of-our-online-study/
Ce n’est pas non plus une maladie génétique: les enfants des patients atteints de kératocône ne développent pas de KC s’ils ne se frottent pas les yeux. On ne devient donc jamais aveugle en cas de kératocône à condition de respecter cette simple prescription; ne plus frotter ses yeux, et traiter la cause des démangeaisons oculaires qui ont conduit à ces frottements (allergie, position de sommeil, etc.)
Bonjour,
J’ai une question simple dont je n’arrive pas à trouver une réponse claire : peut on devenir aveugle à un stade très avancé de la maladie ?
Ma question est peut-être idiote. Et la réponse est probablement oui mais je voudrai être certaine.
Bonjour docteur
On m’a diagnostiqué une keratocone il ya 3 ans à l’oeil droite sans topographie et on m’a prescris des lentilles rigide et j’en suis satisfait je vois bien avec j’ai récemment aller voir un ophtalmo pour m’inscrire des nouvelle il m’a dit qu’il faut faire une topographie
J’ai fait la topographie il a décelé une keratocone stade 3 et 4 il m’a proposé un cross linking pour arrêter l’évolution de la maladie m’a dit il
J’aimerais savoir docteur ton opinion sur le cross linking est ce indispensable ? Et merci
Votre message traduit la dérive « consumériste » que rencontrent de nombreux patients fraichement diagnostiqués pour le kératocône. Contrairement à ce que l’on vous a peut être laissé entendre, vous n’etes pas atteinte d’une maladie d’origine génétique. Vous avez simplement trop frotté vos yeux. La première chose est donc de cesser définitivement ces frottements, et de modifier éventuellement votre position de sommeil pour ne pas appuyer sur les yeux. Si vous effectuez simplement ces deux préconisations, je peux vous garantir que le kératocône n’évoluera plus, et que vous pourrez même avoir une petite amélioration au moins sur le plan de la topographie cornéenne. Ensuite, pour mieux voir, le plus simple et efficace est l’adaptation de lentilles rigides. Si et seulement si cette adaptation échoue, alors vous devrez éventuellement envisager une intervention de type anneaux par exemple, ou laser (si stabilité documentée, qui veut dire que vous avez bien cessé de vous frotter les yeux). Le cross linking n’a aucun intérêt (pour vous) car l’arrêt de ce qui cause la déformation aboutit à la stabilité de la déformation (c’est aussi simple que cela). Vos cornées ne sont pas très amincies, le kératocône doit être à un stade encore modéré, et peut être est il même possible de vous corriger en lunettes pour l’instant. Je vous conseille comme à tous les patients de prendre vos distances avec tout praticien vous proposant d’entrée une ou plusieurs séries d’intervention dès la découverte du kératocône…
Bonsoir Dr Damien, j’ai 30ans et je viens de savoir que j’ai le kératocone .D’après les résultats de la Pentacam que j’ai fais mon ophtalmologue m’a conseillé de faire kpr+cxl pour mon oeil droite et des anneaux +cxl pour mon oeil gauche et j’ai besoin de votre avis sachant que pachy OD=495/OG=490.
Merci infiniment Docteur de votre réponse rapide.
Mon ophtalmologue me demande de retirer mes lentilles 48 h avant l’intervention. Or vous dites que pour le calcul biométrique il serait préférable de les retirer plus tôt. ( même si dans mon cas ce n’es pas forcement indiqué)
Combien de jours avant ? Je préfère prendre toutes les précautions nécessaires.
Et si je dois reporter des lentilles ,il ne s’agira que d’une seule ? et un port intermittent serait il possible ?
Encore merci !
Le kératocône n’est pas une contre indication à la chirurgie de la cataracte. Il ne rend pas l’intervention plus difficile. En revanche, il exerce un effet sur la précision du calcul de la puissance de l’implant (biométrie), car il rend l’estimation de la puissance optique de la cornée (kératométrie) plus incertaine. Ceci n’est pas un problème car la correction d’un oeil atteint de kératocône est également « incertaine » (il n’existe pas vraiment de correction précise car la déformation de la cornée provoque des aberrations optiques que l’on ne peut pas corriger avec des lunettes, d’où la nécessité du port de lentilles rigides). En fonction du degré de déformation de la cornée, il est toutefois très probable que vous ayiez à reporter des lentilles rigides après l’intervention (la chirurgie de la cataracte ne concerne pas le kératocône). Il suffit de retirer les lentilles quelques jours avant l’intervention, pour limiter le risque infectieux. Pour le calcul biométrique, il aurait théoriquement préférable de les retirer plus tôt, mais puisqu’il sera nécessaire de reporter des lentilles rigides après la chirurgie, il n’est pas forcément très intéressant d’obtenir une mesure précise de la kératométrie.
Bonjour Docteur
J’ai une très forte myopie avec astigmatisme et un keratocone à l’oeil gauche, découvert en 2002, le matin d’une opération programmée de la myopie… qui n’a donc pas pu être réalisée à ma grande déception ! Ayant toujours porté des lentilles rigides, celui-ci n’avait pu être diagnostiqué avant.
Pour info j’avais consulté trois chirurgiens, dont deux prescrivaient d’enlever les lentilles l’un une semaine, l’autre trois jours avant l’opération. J’ai choisi le troisième qui préconisait un arrêt de trois semaines, ce qui m’a paru plus sérieux … et s’est vérifié.
Je dois me faire opérer de la cataracte en janvier … après cette mésaventure, j’appréhende les suites de l’opération..
Questions :
Suis je assurée que le keratocone n’est pas une contre indication à l’opération de la cataracte, et celle-ci nécessite-t-elle des précautions particulières ?
J’ai une douleur à l’oeil gauche, quand j’enlève mes lentilles et retrouve mes lunettes avec prisme (pour corriger une diplopie apparue depuis un an)
Combien de temps dois je enlever mes lentilles avant l’opération ?
Merci beaucoup Docteur pour votre réponse … et pour cet inappréciable forum !
En cas de découverte récente d’un kératocône il faut:
– cesser de se frotter les yeux, définitivement, ce qui implique de bien identefier les mouvements impliqués et les moments concernés (matin au réveil, douche, ordinateur, etc.)
– modifier sa position de sommeil si elle fait que la tête « appuie » sur l’oreiller au niveau d’un oeil ou des deux (position sur le ventre ou sur le côté à éviter ou adapter).
– envisager une adaptation en lentilles: meilleur méthode de correction de la vision chez les patients atteints de kératocône
– se méfier des propositions de chirurgies un peu hâtives qui n’ont pas, souvent d’intérêt (pour vous). L’arrêt des frottements permet de stabiliser la déformation, et les gestes comme le CXL ou les anneaux peuvent avoir des résultats incertains ou décevants.
Bonsoir Docteur Damien,
Je viens de découvrir que j’ai le Keratocone sur les les deux yeux avec une forte myopie . Le médecin au maroc m’as conseillé de faire les lentilles ICL Torique. Je ne sais pas quoi faire, est ce je fais l’opération ou bien je met juste les lentilles que je me sens pas à l’aise avec. Pour info Docteur je met maintenant des lentilles souples. Merci pour votre compréhension et je suis honorée de vous écrire.
Bonjour Docteur,
On m’a diagnostiqué un Kératocône bilatéral il y a 3 ans avec un stade plus avancé à l’oeil gauche (myopie) (aucune évolution sur l’oeil droit). un cross linking a été réalisé sur les deux yeux. Suite à cela, j’ai développé un haze à l’oeil droit qui m’a troublé la vue. Grâce à des gouttes cortisonées j’ai retrouvé une acuité normale.
Depuis 1 an ma vue se dégrade à droite avec l’apparition d’un astigmatisme de plus en plus fort
Je ressens une gêne localisée à l’oeil (sensation de voile) et l’ophtalmologue a constaté que l’haze était toujours présent.
Mes questions :
– Est-ce que cet haze peut être responsable (au moins en partie) de l’astigmatisme ?
– Il est présent depuis 3 ans, peut il encore partir ?
– Au niveau de la position de sommeil, j’essaye de dormir sur le dos au maximum mais il m’arrive de bouger dans la nuit. Pensez-vous qu’une seule nuit avec une mauvaise position suffit à déformer la cornée ? (Je ne vois que ça comme explication dans mon cas sachant que je ne me frotte plus du tout les yeux)
Merci par avance pour vos réponses et merci pour votre travail
Rien n’est plus efficace et logique que ce cesser de se frotter les yeux et les protéger éventuellement la nuit. Le terme « logique » est ici employé dans sa dimension scientifique et éthique; dans le cadre d’une logique plus commerciale, il peut être intéressant de proposer aux patients atteints de kératocône tout un tas de thérapeutiques souvent aussi inutiles que coûteuses.
Vous avez bien fait de refuser le cross linking et considéré qu’il était bien plus pertinent de ne plus vous frotter les yeux; il existe des lentilles rigides de différent diamètres pour adapter les cornées atteintes de kératocône (si tel est le cas : le terme de « kératocône léger » ne veut pas dire grand chose). Il est ainsi peut être possible de vous adapter avec des lentilles souples toriques, plus confortables.
Il est avant tout indiqué que vous réalisiez une topographie cornéenne et que vous la compariez avec celles effectuées dans le passé au niveau de l’oeil droit. Il existe d’autres causes de baisse de vision que le kératocône. Concernant l’oeil gauche, frottiez vous particulièrement cet oeil dans l’enfance? Si tel était le cas, la théorie mécanique explique au moins l’atteinte de ce côté. Dans mon expérience (étendue avec le kératocône), les formes unilatérales ou très asymétriques s’expliquent invariablement par l’exercice de frottements et de compression nocturne également unilatérales du même côté. Le fait que le kératocône puisse concerner un seul oeil est d’ailleurs une particularité qui plaide en faveur d’une origine « locale ». A propos de votre oeil droit, le diagnostic de KC n’a peut être pas été retenu dans le passé, ce qui ne veut pas dire que la topographie était complètement normale de ce côté (les patients qui se frottent les yeux le font généralement de manière bilatérale, même si un côté peut être plus concerné, généralement en rapport avec la position de sommeil). Au demeurant, il est probablement vain de chercher une autre cause que traumatique (les frottements) pour expliquer le kératocône. Cette affection est liée à une déformation cornéenne permanente, et toute déformation requiert l’exercice d’une force appliquée localement. La pression intraoculaire (son différentiel avec la pression atmosphérique) constitue la force principale à laquelle est soumise le tissu cornéen. Or, certaines affections qui se caractérisent par un « ramolissement cornéen primitif » (ex le syndrôme de Marfan) provoquent, en l’absence de traumatisme extérieur, un tableau topographique opposé à celui du kératocône (aplatissement global par distention progressive). Les atteints focales du kératocône (amincissement isolé à la région centrale de la cornée et irrégularités de courbure adjacentes) s’expliquent très bien par les frottements…
Bonjour docteur
Que penser vous des nouvelles techniques de correction et stabilisation ,mosaic avedro ,ainsi que la correction avec des ondes courtes..
Merci.
Bonjour Docteur,
Votre hypothèse étiologique du Kératocône est très tentante. Toutefois, mon cas semble s’inscrire en faux avec celle-ci. On m’a diagnostiqué un kératocône à l’oeil G à l’âge de 26 ans qui a été opéré d’un cross-linking 7 ans plus tard. L’évolution s’est après cela stabilisée, voire même, a bénéficié d’une légère amélioration, jusqu’à l’âge de 39 ans, puis la vue s’est à nouveau dégradée, en lien, semble-t-il, avec une opacification de la cornée. L’autre oeil avait jusqu’alors été épargné, mais je constate depuis quelques mois, à l’âge de 43 ans, la survenue de symptômes similaires à ceux qui m’avaient alerté pour l’oeil gauche. Un ophtalmologue avisé avait attiré, voici plus de 10 ans, mon attention sur les facteurs de risques mécaniques aussi ai-je veillé à ne jamais, ou rares exceptions, me frotter les yeux, ainsi qu’à les hydrater 3 à 4 fois par jour. De même ai-je pris la précaution de les protéger systématiquement du soleil.
Si, comme vous le supposez dans cet article, l’origine du kératocône se veut purement mécanique, je n’aurais pas dû être affecté au niveau de mon oeil sain. N’êtes-vous pas d’accord?
Bien cordialement
Bonjour à mon dernier rendez-vous suite à une baisse de ma vue forte myopie et forte astygmatie
OD -675(-3.50) 10°
OG-7. 50(-3.25) 160°. On m’a fait une topographie et la on me dit keratocone léger OD et OG. Essai lentilles rigides (menicon ZD et rose k2 en -3) mais je n’y voyait rien. À la suite de ces 2 essai on me propose un cross Linkin. Que je n’ai pas fait. Je me suis beaucoup gratter les yeux étant jeunes mais plus maintenant j’evite au maximum. Existe t il d’autres modèle de lentilles ? Mes verres sont très épais
Vous avez raison car si l’on n’explique pas au patient qu’il ne faut pas se frotter les yeux trop vigoureusement et souvent (quelle que soit la cause des frottements), le risque de voir un kératocône apparaître est accru: le kératocône, comme vous l’avez compris en lisant les pages de ce site, est provoqué par l’action répétée des frottements. Cette théorie est très compatible avec les observations du monde réel, mais elle n’est pas communément reconnue comme valide par la communauté opthalmologique… poids des dogmes, et parfois malheureusmement conflit d’intérêt avec la pratique de certaines interventions comme le cross linking.
Il convient de vérifier que vous ne dormez pas sur le côté ou le ventre en appui avec la tête sur un oeil ou les deux (contre le matelas, la main, l’oreiller…). Ces habitudes de sommeil sont fréquentes chez les patients atteints de kératocône.
Bonjour, docteur
Je voudrais savoir, j’ai eu les lentilles rigides, le cross liking, les anneaux, et ma vue change suivant mon sommeil en bien ou en mal.
Ce matin j’ai etait a la visite medicale du travail pour valider mon caces et j’ai 6/10 binoculaire. Quesque vous me conseiller? Merci d’avance
Bonjour, je fais plein de recherches actuellement sur le keratocone car je v me faire opérer le 18/10.
Je lis notamment qu’il serait dû aux frottements et à la sécheresse des yeux.
En effet, je me rends compte que je me frotte souvent les yeux et ce depuis justement le port de lentilles depuis 25 ans maintenant. Je ne les supporte plus. C’était des souples.
Je pense que mettre des lentilles rigides n’arrangerait rien pcq quand on les enlève, on a besoin de se frotter les yeux !
Je pense donc que j’avais sans doute à la base une cornée plus fine mais que c’est donc le port de lentilles pdt toutes ces années qui ont fait en sorte que j’ai ce keratocone apparaisse !
Je pense donc que porter des lentilles rigides améliore sans doute la vue avec un keratocone mais continue à l’accentuer vu la sécheresse et le besoin de se frotter les yeux après les avoir enlever.
IL est crucial de ne plus frotter vos yeux, et si le traitement prescrit vous permet de calmer les démangeaisons et irritations locales, alors il est conseillé et ne représente aucun danger pour les yeux. Un suivi régulier avec réalisation de cartes topographiques permettra de confirmer la stabilité du kératocône.
Bonjour Docteur
Je suis atteint de keracotone des deux yeux stade 1 et 2
Je porte des lunettes ,je me frotte plus les yeux depuis 2 ans
Je n’est pas fait le CLX,c’est que je n’est pas arrêté d’utiliser un collyre humidifiant que j’utilise pour éviter les frottements ,ma question est ce que ça peut nuire à mes yeux. Merci
Toutes les activités sportives peuvent être exercées en cas de kératocône: il est simplement très déconseillé de se frotter les yeux vigoureusement en cas de transpiration, projections, etc.
Salut Dr. Est ce qu’on peut pratiquer la musculation quand on est au stade 2 OD et 3 OG du kératocône ??? MERCI D’AVANCE
Il faut simplement éviter tous les facteurs qu pourraient vous conduire à vous frotter les yeux de manière excessive et vigoureuse. La vapeur ou la chaleur ne sont pas en soit un souci, si vous ne vous frottez pas/plus les yeux.
Un amincissement cornéen isolé sans augmentation de la déformation est peu vraissemblable. Il s’agit probablement d’un artéfact de mesure. Il serait utile de vérifier la réalité de cet amincissement en réalisant un nouvel examen, avec le même instrument si possible que lors de la précédente mesure d’il y a quelques mois si ce n’était pas le cas. Il est crucial de comprendre et tenir compte de la variabilité des examens pour le kératocône; la répétabilité est moindre que pour les cornées normales. Une variation de kératométrie inférieure à 1D n’est pas statistiquement significative pour les formes avérées de kératocône. Ironiquement, la plupart des études concernant le CXL rapportent une évolution tardive de la kératométrie de l’ordre d’une réduction d’une demi dioptrie… Ce qui non significatif. Par ailleurs, il ne sert à rien de tenter de durcir une cornée dont la déformation n’est pas primitivement causée par une perte de la rigidité « spontanée ». Une cornée « molle » mais non frottée s’amincit et s’aplatit au fil du temps, comme l’enseigne l’étude du syndrome de Marfan. Dans le kératocône, la cornée se cambre de manière irrégulière, car les frottements lèsent principalement la région centrale de la cornée. Cette perte focale de la rigidité explique le caractère particulier de la déformation cornéenne : amincissement centrale et déformation permanente avec cambrure centrale et aplatissement périphérique. Pour enrayer l’évolution du kératocône, il est nécessaire et suffisant de ne plus frotter du tout, et modifier éventuellement sa position de sommeil.
Bonjour docteur,
Je sors de mon deuxième rendez vous chez l’ophtalmologiste à 3 mois d’intervalle. La déformation cornéenne de mon œil droit n’a pas évolué durant ces quelques mois mais l’épaisseur de ma cornée elle a diminué. J’étais à 520 micron et je suis tombé à 470. La recommandation du praticien est donc de pratiquer un cross linking sans attendre, en effet il semblerait qu’elle ne souhaite pas opérer des cornées plus fines que 450 microns . Je suis un peu perdu. Si le but de cette intervention est de durcir la cornée pourquoi est elle utilisée pour ce problème d’amincissement ? Je comprend bien que de manière générale le cross linking n’est pas votre recommandation de toute façon. A noter que durant ces quelques mois j’ai réduit les frottement. Je ne peux pas dire que je ne le fais plus jamais mais très rarement.
Bonjour Docteur,
Fin 2015 (19 ans) j’ai découvert que je me suis atteint d’un Kératocone pour les deux yeux.Mon médecin m’as conseillé de porter des lentilles rigides mais je les pas supporter.En 2017 je me suis oppéré par l’operation Crosslinking et puisque je n’est pas supporter les lentilles j’ai fait une lunette qui ne m’aide vraiment pas.Maintenant je travaille dans un restaurant ou la chaleur est forte et la vapeur aussi.
Ma queston est-ce que il faut que j’évite la vapeur et la chaleur !?
Malheureusement, la réalisation du CXL expose à des complications cicatricielles, inflammatoires ou infectieuses (environ 10 à 15% des cas). Si vous lisez ce site, vous comprendrez que son auteur ne préconise pas cette technique qui paraît globalement inefficace (la cornée n’est pas durcie) et finalement pas justifiée quand on réalise que la cause du kératocône est mécanique (frottements oculaires excessifs). Même si la cornée était un peu durcie par le CXL, ce durcissement serait trop faible vis à vis de la force délivrée par les frottements oculaires (il faut tout de même plusieurs années de frottements, en général, pour qu’un kératocône, c’est à dire une déformation permanente de la cornée, apparaisse). IL est nécessaire de suivre la cicatrisation de la cornée de votre frère de manière rigoureuse. La vision devrait baisser pendant quelques semaines, avant de revenir à son niveau d’avant le CXL (une petite amélioration est parfois observée: elle n’est pas spécifique à la technique, car elle relève de la régularisation cicatricielle que l’on observe parfois quand on « stimule » la repousse de l’épithélium cornéen – celui ci est retiré au début de la précédure du CXL).
Bonjour Docteur
Mon frère est atteint d’un kératocône bilatéral ( stade 2 OG et 4 OD ), diagnostiqué vers 22 ans , associé a un astigmatisme irrégulier
Il a subi un crosslinking à chaque oeil à 3 jours d’intervalle. Il lui avait été dit qu’avec le crosslinking, le keratocone se stabiliserait.
4 jours après l’opération des taches blanches sont apparus au niveau de la cornée (2/3 de la pupille ) avec une image flou et incomplète juste après une inflammation oculaire intense qui a persister 24 h
je sais pas exactement la cause de ses taches et s’elles vont disparaître par des antibiotiques habituelle ( si c une infection ) ou ça nécessite une autre opération ( Photokeratectomie thérapeutique par exemple ) ?
il prend maintenant :
– Thealose
– Vigamox
– Dexafree
N’ayez crainte, cette théorie est malheureusement juste ;-) Toutefois, le bon côté de la médaille est que la cessation des frottements garantira l’absence de progression de la déformation cornéenne (qui est mineure et le restera donc). La projection d’un corps étranger dans l’oeil ne fait pas progresser le kératocône/la déformation. Ce dernier correspond à une déformation qui reqiuert beaucoup d’énergie cumulée. La présence d’un corps étranger, si elle n’est pas source de frottement, pourra provoquer une inflammation locale isolée et qui disparaîtra en principe avec le retrait de celui-ci. Dans ce genre de circonstance, il est toujours préférable de rincer les yeux plutôt que de les frotter.
Bonjour Docteur,
Je me suis atteint de kératocone (uniquement visible sur une topo), j’ai donc un astigmatisme irrégulier qui me dérange surtout la nuit lorsque je regarde, par exemple, des feux arrières de voitures (vision triple ou double).
Depuis ma visite sur votre site j’arrête tous frottements oculaires. En effet je me grattais beaucoup les yeux à cause de mes allergies. De plus je travaille dans un milieu avec beaucoup de poussière (BTP) qui me donne souvent envie de me gratter les yeux. J’ai aussi arrêter de dormir sur le ventre.
J’espère que votre théorie est juste.
Je voulais, cependant, avoir une information. Si je reçois un grain de sable ou une poussière épaisse dans l’oeil, est ce que cela peut créer une évolution du KC si cela n’est pas retiré rapidement?
Je vous remercie pour votre intérêt.
Merci pour votre réponse…Je vais me diriger vers le centre des keratocones de Bordeaux ou Toulouse..
Scleral lenses are a good option for eyes with keratoconus which cannot be fitted with rigid CLs. Instead of trying CXL, which does not address the real cause of KC, you should truly focus and concentrate your efforts toward the cessation of eye rubbing. Rubbing exacerbate local irritation and trigger further corneal deformation. Scleral lenses sometimes help to relieve the itching and irritation because the ocular surface is immersed in saline solution.
Le but supposé du CXL est de durcir la cornée, car la plupart des ophtalmologistes considèrent le kératocône comme une pathologie liée à une défaillance biomécanique « spontanée » de la cornée. Si vous lisez les pages consacrées à ce sujet sur ce site, une autre conception du kératocône, qui est beaucoup plus corrélée à la réalité clinique constatée de manière quotidienne, fait de cette affection une pathologie d’origine mécanique: les frottements oculaires excessifs provoquent la défaillance biomécanique de la cornée (d’autant plus rapide que les frottements sont intenses, répétés, prolongés et que la cornée est initialement fine). Aussi, la stabilisation du KC peut être « simplement » obtenue par l’arrêt des frottements (et éventuellement la modification de la position de sommeil quand elle provoque une compression oculaire nocturne prolongée). Au cours de la grossesse, la sécheresse oculaire augmente notablement, et ceci conduit parfois à l’exacerbation des frottements oculaires, d’où la progression constatée. Après la réalisation d’un CXL, la cornée est sensible et il est généralmeent observé un arrêt de frottements (ce qui constitue au moins un bénéfice pour cette techique). Pour le reste, la cicatrisation peut être difficile, le taux de complications (incluant le retard cicatriciel) est estimé à 15% après CXL. La cornée, déjà traumatisée sur le plan mécanique, subit alors, au cours du CXL, un traumatisme photochimique… La cicatrisation épithéliale peut modifier ensuite légèrement la courbure de la cornée. Il faut attendre quelques mois pour juger de la stabilité. Le cacicol est supposé accélérer la cicatrisation épithéliale. Ce traitement est un peu couteux et prescrit dans les cas de cicatrisation difficile. Les cornées fines sont de mauvaises candidates au CXL car cette technique fait courir un risque pour l’endothélium de la cornée (les UV sont toxiques pour les cellules endothéliales quand celles ci ont été imprégnées de riboflavine). Mais comme vous l’aurez compris, ce n’est pas de mon point de vue un souci majeur, et presque une « chance » qu’il ne soit pas possible d’effectuer un CXL chez vous, car je considère que cette technique, dont l’efficacité en matière biomécanique est douteuse, n’est de toutes façons pas une bonne réponse au problème que pose le kératocône.
Il existe chez certains chirurgiens une certaine propension à proposer ces techniques chirurgicales. Le CXL a pour but (théorique) de durcir la cornée, mais si vous suivez ce site, vous savez que le problème en matière de kératocône n’est pas de durcir la cornée mais d’arrêter les frottements oculaires qui sont la cause de la déformation cornéenne permanente que l’on appelle « kératocône ». Même si la cornée durcissait après le CXL, ceci serait de toutes façon insuffisant pour freiner le KC en cas de frottements (la force véhiculée par les mains est bien plus importante que les capacités de résistance d’un tissu biologique même modifié soumis à un stress physique répété). Les constatations effectuées après CXL in vivo (sur des patients et non en laboratoire sur des morceaux de cornées) ne révèlent pas de durcissement probant, voire pour certaines études, plutôt un « ramollissement » (!) Le CXL est toujours proposé car il est difficile de revenir sur une technique source de revenus, et souvent demandée par les patients puisqu’elle leur est présentée comme une solution à leur problème et angoisse de progression. Les anneaux ont eux pour but de réduire la déformation de la cornée pour essayer de réduire l’astigmatisme et améliorer un peu la vision. Ils ne permettent toutefois pas de se passer de lunettes ou lentilles (l’adaptation des lentilles peut d’ailleurs être rendue plus difficile par la présence des annneaux). Enfin, le laser est souvent utilisé pour améliorer la vision au delà de l’effet des anneaux… Le gain (médical) attendu est souvent perçu comme un peu décevant par les patients. Le meilleur moyen d’améliorer la vision d’un oeil atteint de kéraotcône est l’adaptation réussie d’une lentille (rigide, ou sclérale pour les déformations prononcées).
Bonjour
Je suis atteint de kératocone sur les deux yeux depuis 5 ans un de vos confrères me propose crosse linking plus anneaux plus laser sur anneaux si besoin je vous suis depuis lomgtemp et ne frotte plus mes yeux en revanche ma vue baisse d’année en année qu’en pensez vous.??
Merci pour le temps consacrer
Bonjour Docteur,
Je suis atteinte d’un keratocone et il ne cesse d’évoluer surtout pendant mes grossesses (2014-2017) mon ophtalmo a finalement opté pour un CXL que j’ai eu le 1 juillet. Etant loin de mon ophtalmo j’ai du suivre la cicatrisation chez un autre ophtalmo en attendant mon Rdv de contrôle du 30 , ce dernier a mis en cause toute la procedure de mon CXL d’ou mes questions suivantes:
-est ce normal qu’ a j12 la cornée n’est toujours pas cicatrisé?
– combien de temps faut-il attendre avant d’adapter une nouvelle correction a l’oeil opéré ?
– le calcicol est-il administré dans mon cas?
– l’epaisseur De ma cornée gauche est inférieure a 400u donc le CXL n’est pas la solution adéquate quel est l’alt?
Merci bien pour toutes les précisions apportées par vos soins.
First of all a massive thank you Dr Damien Gatenil . I am 23 years old I am suffering from a sever allergy in my eyes since i was a child so it has become abvious that rubbing my eyes causes me keratoconus . i am using rigide lenses for 3 years the vision becames clear as i did cross linking on my right eye and I supposed to do the left eye too, but I couldn’t because it’s been 1 year now and that eye still hurts and can’t handle the lense anymore and it kinda became dry with a cloudy vision . i am wondering if the scelar lenses would be better for my eyes than the rigid? , I am afraid to do the cross in the other eye!! , i am aware of rubbing envolve the cornea but honestly I can’t stop myself… ALL the eye drop I’ve used don’t soothe my eyes. what should I do Dr I really need your help because i am in a country where i went to the best professors but in vain
Bonjour Dr Gatinel
Porteuse de deux keratocones qui se sont stabilisés, je dois prochainement subir une coelioscopie pour kyste ovarien. Cette intervention ne peut elle avoir un impact négatif ( pression) sur l’évolution de mes kc ..? Et aussi , que penser des conséquences que peut avoir l ‘IRM sur la vision des patients atteints de kc ?
Avec tous mes remerciements.
Il paraît effectivement souhaitable que vous puissiez réaliser un nouvel essai avec les nouvelles génération de verres scléraux.
Une sensation de baisse visuelle ne traduit pas forcément l’évolution du kératocône. Dans certaines situations, la surface oculaire (film lacrymal) peut être altérée, pour des raisons liées au kératocône, ou à des pathologies associées (blépharite), voire les conséquences de la réduction de la sensibilité cornéenne provoquée par le cross linking. Ce ne sont pas les pauîères qui sont responsables de traces rouges sur le « blanc de l’oeil ». La pression exercée par les paupière est de plusieurs ordres de magnitude inférieure à celle qu’infligent les doigts lors des frottements. Il est par ailleurs essentiel que vous ayez pu arrêter les frottements et modifier votre position de sommeil. Si vous respectez ces consignes, le KC n’évoluera pas, car la déformation cornéenne n’est pas initiée de manière spontanée, du moins dans les formes débutantes à moyennes.
Bonjour Docteur,
j’ai été diagnostiqué d’un kératocône en Septembre 2016, après avoir remarqué une baisse de vision sur l’oeil gauche. J’ai subi un cross linking à chaque oeil, même si l’oeil droit ne présentait pas à l’époque d’évolution.
Suite à la découverte de la maladie, j’ai arrêté immédiatement tout frottement sur les yeux et je dors désormais exclusivement sur le dos. Je suis extrêmement attentif à cela surtout après avoir lu votre site.
Cependant, malgré toutes ces précautions, je remarque désormais une dégradation sur l’oeil droit. Je suis étonné car d’après toutes vos réponses vous semblez persuadé que toute évolution est liée aux frottements oculaires.
Comment expliquez vous cela ? Pensez vous que les paupières peuvent avoir un rôle dans la déformation de la cornée, avec un impact certes minime mais continu tout au long de la journée. Je remarque notamment que ma cornée est marqué par ma paupière inférieure (trace rouge)
Merci par avance de votre reponse.
Merci également pour tout votre travail en faveur des patients atteint de kératocône.
Bonjour Docteur
J’ai été greffé en 1975 puis 1976 par le professeur Pouliquen puis en 1995 et 1996 par le professeur Colin pour une récidive
Ma vue a rebaissé depuis
Madame Mallet a tenté de m’équiper en lentilles toriques en 1996, elle obtenait 10 aux deux yeux mais malheureusement si pour un oeil le confort était parfait, pour l’autre, le greffon étant légèrement décentré le port devenait insuportable au bout d’une heure
Pensez-vous Docteur que les nouveaux verres scléraux pourraient m’apporter une solution.
J’ai été équipé dans les années 70 par le Docteur Cochet de verres scléraux (ancien modèle) quand je ne supportait plus les lentilles rigides suite à l’évolution du Kératocone.
Mais le port de ces verres n’était pas très agréable.
Merci de l’attention que vous portez à la maladie du kératocone.
Dominique Derrien
Le but de la chirurgie par pose d’anneaux vise à réduire l’astigmatisme et permettre une correction lunettes ou lentille. Si la pose d’anneaux intra cornéens ne vous permet pas de mieux voir, ni d’être corrigé en lentille ou lunettes, alors ils ne servent à rien ou pas grand chose. Espérons que l’adaptation d’une lentille de contact pourra vous rendre une meilleure vision; toutefois, sachez que la pose d’anneau peut compliquer l’adaptation d’une lentille rigide. En principe, tout kératocône doit d’abord faire l’objet d’un essai de lentilles, car les lentilles sont les dispositifs qui corrigent le mieux la vision des patients atteints de kératocône. Malheureusement, certains praticiens sont très interventionnistes et orientent les patients atteints de kératocône vers des opérations chirurgicales pas toujours utiles…
Bonjour Docteur Damien,
Je vous remercie pour les informations que vous avez mis dans votre site !
Je viens de faire des anneaux intra cornéens au niveau de l’œil gauche. D’après mon médecin mon keratocone est décentré. Ça fait15 jours de l’intervention mais toujours pas d’amélioration visuelle, aussi je commence à sentir une douleur au niveau de contour de l’œil et aussi une fatigue. Ma question est ce que je peux porter des lunettes ou bien des lentilles sachant mon médecin m’a dit c’est impossible de corriger la vision avec les lunettes.
Salutations,
La musculation n’est pas contre indiquée. Ce qui l’est, ce sont les frottements oculaires. En cas de transpiration du visage, veillez à ne pas frotter vos yeux et essyez le visage délicatement.
Bonsoir Dr; est ce que la musculation est contre indiquée en cas du keratocone stade 2/3 ?
Mercii
Bonjour Docteur,
J’ai 27 ans et un kératocône ayant commencé à évoluer vers 19-20 ans. J’ai actuellement un astigmatisme léger à modéré à chaque oeil (-1,75 ou -2..). Je ne porte ni lunettes ni lentilles, par choix. Lunettes uniquement par sécurité en voiture. A long terme, est-il néfaste pour le cerveau de recevoir des stimulations visuelles de mauvaise qualité, c’est-à-dire sans correction visuelle ? Je commence à accepter petit à petit la baisse de ma vision, à faire le deuil de ma vue d’avant (j’ai suivi vos conseils sur les frottements et espère ainsi garder une stabilité cornéenne) mais j’ai peur qu’au fil des années la mauvaise qualité de ma vue ait une influence sur les zones cérébrales visuelles et plus largement sur le cerveau en général… Je pense notamment aux démences. Dans mon quotidien je suis gênée chaque jour par mes difficultés visuelles (perte des contrastes++) mais parviens à les compenser assez efficacement du fait de mon âge et d’un mode de vie assez routinier.
Je vous remercie Docteur pour la précision de vos réponses ainsi que le partage de vos connaissances pour le bien des patients.
Bonjour Docteur,
Je vous remercie pour vos éléments.
Pour les frottements, mon conjoint est bien au fait et ne se frotte plus les yeux. D’ailleurs, dès qu’il voit quelqu’un se frotter les yeux, il l’informe des méfaits…
Donc, si je comprends votre réponse, vous proposez de changer la position du sommeil en dormant sur le dos et l’essai de lentilles verre scléral?
Je vous remercie par avance.
Il existe des cas de concordances entre jumeaux, commme dans le cas que vous rapportez. Ceci ne démontre pas grand chose, si ce n’est qu’il existe probablement un terrain identique (cornée fine et/ou atopie), et un environnement identique si les jumeaux ont été élevés ensemble. Ainsi, deux jumeaux aux cornées un peu fines et se frottant les yeux devront développer chacun un kératocône. Si vous exposez deux jumeaux à la même dose de rayonnement solaire UV, il développeront un coup de soleil, et ceci bien sûr ne signifie pas que le coup de soleil est une affection primitivement génétique. Si les jumeaux ont un phototype clair, ils auront plus de risque de développer un érythème après exposition. Il existe par ailleurs de nombreuses observations de cas de discordances entre jumeaux monozygotes pour le kératocône; un jumeau atteint, pas l’autre. Un seul cas de discordance (et il y en a beaucoup) chez des jumeaux monozygotes prouverait que le KC n’est pas une affection primitivement génétique! Rapplons pour finir que seulement 10% des KC sont familiaux, le reste étant constitué de cas « sporadiques » Dans une fratrie ou seul un élément a un KC, on note généralement qu’il s’agit de l’enfant qui était allergique, se frottait les yeux, etc.
Le facteur qui déclenche et entretient l’évolution du kératocône est la réalisation de frottements oculaires répétés. Quand on regarde un écran de manière prolongée, il peut y avoir une fatigue oculaire, un désèchement (moins de clignements), et tout ceci peut induire l’envie de frotter. Il faut enrayer ceci si vous voulez être certain qu’il n’y aura pas d’évolution péjorative.
Si le kératocône évolue, c’est que votre conjoint n’a pas cessé de se frotter les yeux, ce qui est effectivement difficile en cas de poussée allergique. Il existe des lentilles spéciales, de type « verre scléral », qui sont souvent plus confortables une fois l’adaptation réalisée (ces lentilles sont conçues pour être remplies de sérum physiologique pour favorise une meilleure vision et hydratation oculaire).
Il convient de réaliser une topographie cornéenne qui servira de référence. Sur ce site, ainsi que celui-ci: http://www.defeatkerartoconus.com, vous trouverez de nombreuses informations sur le KC. En bref, il convient que les frottements oculaires cessent définitivement (ils sont la cause de la déformation) et la position de sommeil, si elle induit un appui sur l’orbite (sur le ventre ou le côté avec tête contre l’oreiller), doit être modifiée. Si ces deux prescriptions sont réalisées, il n’y aura pas de progression, et une correction en lentilles (rigides) pourra être réalisée.
Pour stopper l’évolution du kératocône, il suffit d’obtenir l’arrêt des frottements oculaires, et dans certains cas, de modifier la position de sommeil pour éviter les appuis nocturnes prolongés sur l’oeil. Si un cross linking est réalisé et que les frottments se poursuivent, cela ne servira à rien. Après le CXL, la douleur et la cicatrisation font que les patients cessent de se toucher l’oeil, et c’est de cette manière que la déformation cornéenne cesse d’évoluer. Il suffit de ne plus se frotter les yeux, sans CXL, et il n’y a plus d’évolution. La pose d’anneau est indiquée pour réduire l’astigmatisme cornéen, et peut être faite quand les frottements on cessé.
Bonjour docteur
En mars 2018 les docteurs ont diagnostiquer un KERATOCONE chez ma fille, il était au stade 1, la solution préconisé était les lentilles semi regides du fait que ma fille n’a pas pu tolérer des lentilles regides après une année son KERATOCONE s’est vu évoluer au stade 2, maintenant les médecins préconisent un cross linkikg, ma question est dois-je au préalable faire insérer un anneau intra corneens ensuite un cross linking ou cela importe peu et on peut faire l’anneau par la suite, car d’après son médecin traitant l’urgence est de stopper la maladie
Merci
Cordialement
Bonsoir docteur,
Il y’a 6 ans on a diagnostiqué chez ma femme – 39 ans- un keratocone bilatéral depuis on l’a pas contrôlé jusqu’à hier, stade avancé et sévère oeil droit 0.5/10 et e gauche 6/10 avec lunette côté droit 4/10. Qu’elle est la conduite à tenir? Que faut-il éviter? Sachant qu’elle est medecin et utilise quotidiennement l’échographie.
Merci
Bonjour Docteur,
Mon conjoint est atteint d’un kératocone bilatéral, dignostiqué vers 35 ans (il y a une dizaine d’années), associé à une dispersion pigmentaire ( diagnostique en 2015).
Il a subi un crosslinking à chaque oeil à un an d’intervalle. Il lui avait été dit qu’avec le crosslinking, le keratocone se stabiliserait. Mais ce n’est pas le cas.
Pour la dispersion pigmentaire, il a subi une intervention au laser sur un oeil. Il ne souhaite pas se faire opérer du second, car depuis l’opération, il voit un « trou » et pas d’autre amélioration…
Il a essayé les lentilles rigides, qu’il ne supporte pas: difficultés à la pose et au retrait, perte dans l’oeil, et une fois les lentilles posées, ses yeux « s’injectaient » de sang.
Il a consulté en centre hospitalier universitaire et en cabinet privé, le bilan à ce jour: nous ne pouvons rien faire pour vous si vous ne supportez pas les lentilles!
Aujourd’hui, il porte des lunettes, qui l’aident à améliorer la vision mais ce n’est pas une correction à 100%. On parle d’une amélioration de 25-30%…
De plus, il a l’impression que la maladie évolue à chaque crise allergique.
Que pouvez-vous me conseiller?
Je vous remercie par avance de votre réponse.
Bonjour M, j’ai un Kératocône évolué dans l’œil gauche j’ai fait un cross licking sur cet œil. est ce que les écran (TV,PC,Téléphone) peuvent influencer sur l’évolution de cette maladie surtout au niveau du l’œil opéré ?
Je me demande si votre hypothèse est plausible dans le cas de mon compagnon (29 ans) qui a été diagnostiqué tardivement du keratocone. (2013) Il a effectué en urgence toutes les procédures qui ont été vaine au Quinze Vingt. Le plus curieux est la maladie partagé par son frère jumeau. (Vrais jumeaux)
Comment pouvez vous expliquer ce phénomène ?
Il est probable que votre kératocône a un peu évolué. Dans notre expérience, l’évolution est contingente de la réalisation de frottements oculaires répétés et particulièrement vigoureux; il est crucial de ne plus frotter les yeux pour stabiliser la déformation cornéenne. Si vous dormez sur le ventre ou le côté, il faut aussi modifier ceci pour éviter toute compression/chaleur/irritation oculaire, qui généralement déclenche aussi l’envie de frotter. Il suffit de peu d’astigmatisme pour induire une gêne visuelle empêchant de voir net de près et de loin. Les lentilles sclérales sont un excellent moyen de correction optique, mais elle exigent certaines contraintes.
Bonjour Docteur,
Mon kératocône a été détecté à l’age de 16 ans mais ne nécessitait pas de port de lentilles. Je voyais bien et pouvais tout faire sans lunettes. C’est lorsque ma vue a commencé a baissé et à ne plus être corrigée par les lunettes que je me suis résolue au port des lentilles à l’age de 30 ans (j’ai actuellement 34 ans).
J’ai tout d’abord essayé les petites lentilles rigides, mais je n’arrivais pas à les mettre ou les perdais dans l’oeil. J’ai ensuite essayé des lentilles mi souple-mi rigides, puis des lentilles sclérales rigides pour lequelles mon opthalmologue et moi avons opté.
Effectivement ma vue était bien meilleure qu’avec les lunettes (quasi 10/10) par contre mon gros problème c’est que sans les lentilles je ne vois plus rien. C’est arrivé dés le début donc je ne pense pas que mon oeil se soit habitué si vite. Moi qui pouvait tout faire sans lunettes je suis devenu complètement dépendante. J’aimerais savoir pourquoi? Est ce que cela arrive fréquemment? Mon opthalmologue pense que c’est normal et que je vois tellement mieux avec les lentilles que j’ai l’impression qu’il y a une énorme différence. Ce n’est absolument pas le cas. Pour exemple: avant les lentilles je voyais sans problème le compteur de mon VTT assise sur le vélo, maintenant je ne discerne même plus les couleurs. Je ne peux plus conduire, je ne peux plus rien faire….
Merci d’avance pour votre aide.
Il n’est absolument pas nécessaire de réaliser un CXL pour bénéficier d’une adaptation en lentilles en cas de kératocône, ou de la pose d’anneaux. L’attitude consistant à proposer systématiquement un cross linking a un patient atteint de kératocône est abusive. Comme expliqué sur ce site, le CXL n’a pas vraiment fait la preuve se son efficacité pour freiner le kératocône (les études sont généralement faibles sur le plan statistique, sans groupe témoin, sans évaluation de l’impact de l’arrêt des frottements etc.). In vivo, la cornée n’est pas durcie par le CXL et quand bien même elle le serait, ce ne serait pas suffisant pour contrer l’effet des frottements oculaires qui exercent une force potentiellement bien supérieure au seuil de résistance d’un tissu biologique. Comme vous l’avez compris, les frottements sont l’élément déclencheur et aggravant du kératocône. Leur arrêt est nécessaire et suffisant pour stopper l’évolution de la déformation. Bien entendu, ce « remède » est plus économique (pour le patient), et meêm s’il n’est pas toujours simple à mettre en oeuvre, il revêt une importance cruciale. Traiter les facteurs d’irritations locaux est très important (les cils ectopiques, la sécheresse – cette dernière augmente en effet souvent pendant la grossesse avec recrudescence des frottements).
Il n’est pas recommandé d’exercer une pression sur la cornée en cas de kératocône; les frottements oculaires avec les doigts sont responsables d’une fragilisation avec décompensation biomécanique et altération du galbe naturel de la cornée. Ceci provoque l’astigmatisme initial. La déformation provoquée par un appui chronique est assez imprévisible et pourrait contribuer, par le biais de modifications locales (activations enzymatiques, élévation de la température), à aggraver la situation. Les lentilles hybrides pourraient être une solution dans votre cas (rigides dans leur portion centrale mais souples en périphérie).
Bonjour Docteur,
Je présente un kératocône légèrement/moyennement évolué (au moins -1,75 astig. à chaque oeil) et depuis que j’ai cessé tout frottement (digital) sur les yeux, ma vue s’est stabilisée. Mais j’ai ensuite commencé à porter des lentilles rigides et il me semble que ma vue a de nouveau baissé… Mon prochain contrôle ophtalmo est prévu pour juillet mais je perçois que mon astigmatisme a encore augmenté… Personnellement j’arrête d’utiliser les lentilles rigides car il s’agit tout de même de frottements incessants touchant directement l’oeil.. Je ne présente pas de sécheresse oculaire ni de douleur mais je ressens toujours les frottements liés au déplacement de la lentille sur la cornée. Egalement, les petites poussières (normalement anodines et peu gênantes sur un oeil nu) sont une vraie torture lorsqu’elles passent sous la lentille rigide :O (les porteurs de lentilles rigides se reconnaîtront). Bref j’ai des lunettes que je n’aime pas porter, je les mets uniquement pour conduire, par sécurité. Mon ophtalmo me dit que seules les lentilles rigides ou les lunettes sont possibles dans mon cas.
Y a-t-il une autre solution envisageable d’après vous ? Je n’ai pas non plus le droit à l’orthokératologie car j’ai une légère myopie et que « la différence entre myopie et astigmatisme est trop importante chez moi (je n’ai pas compris ce que ça implique) »
Où en est la recherche concernant la GUERISON des yeux (sans passer par la chirurgie) comment retrouver la santé oculaire de mon enfance ? Je rêve (j’ai espoir) qu’un jour il suffise d’un médicament, d’un collyre, d’exercices de rééducation pour guérir des yeux… Concernant le kératocône, c’est quand même vachement dommage de voir complètement flou juste à cause d’une minuscule cornée capricieuse (je la maudis chaque jour..) et je n’ai pas vraiment l’impression d’avoir un oeil « malade ».. et pourtant l’impact sur le quotidien est énorme.
Y a-t-il une alimentation à privilégier, des aliments à bannir ? J’ai arrêté de manger de la viande et du poisson un peu avant l’apparition du kératocône, c’est peut-être lié… ?
J’en suis même arrivée à envisager ceci : « Les anciens Chinois mettaient de petits sacs de sable sur leurs paupières, la nuit, pour diminuer leur myopie et pour mieux voir durant la journée. C’est une notion classique qui est sans doute une des premières tentatives de remodelage cornéen. » http://www.snof.org/encyclopedie/orthok%C3%A9ratologie-et-crt
Je vais éviter le sable mais j’aimerais tenter la nuit de placer sur les yeux un bandeau pour les yeux, en le serrant légèrement de telle sorte qu’il y ait un très léger appui sur les cornées… ? Cela peut paraître fou mais c’est sans doute moins agressif /invasif que certaines chirurgies non ? Et puis si les chinois le faisaient :-)
Et puis l’impact du stress/de la fatigue/du manque de lumière : c’est un fait je vois beaucoup mieux lorsque je suis au soleil, à l’autre bout du monde et que je suis détendue… (je vis pour l’instant dans une zone très peu ensoleillée, j’ai vraiment l’impression que ça aggrave les difficultés..)
Merci Docteur pour votre compréhension
Bonjour,
J’ai 32 ans et j’ai été diagnostiquée d’un keratocone en janvier.OG est au stade 3 et on m’a parlé de kératocone frustre pour l’oeil droit.
Une topographie cornéenne a été réalisée aujourd’hui et mon keratocone n’a pas évolué depuis le mois de janvier.
En effet, j’ai beaucoup parcouru votre site.Et j’ai complètement arrêté de me frotter les yeux et je dors à présent sur le dos.
J’ai bien prit le temps d’analyser ce que vous dites au niveau des frottements, et effectivement je me frotte beaucoup les yeux:
Avant, je vivais aux antilles et je n’avais pas de problèmes d’allergies.Et voilà huit ans que je vis en France et j’ai commencé à devenir très allergiques aux pollens depuis environ 4 ans.
L’année dernière j’ai subi les allergies durant la grossesse et ne pouvant pas me traiter avec les antihistaminique, je me suis énormément frotté les yeux. Et c’est vers mon sixième mois de grossesse que j’ai constaté que ma vue avait baissé.
Par la suite, cela avait l’air de s’accélérer même apres la grossesse et m’a poussé à consulter en novembre dernier.
J’ai définitivement arrêté de me frotter les yeux mais cela est très difficile à gérer car je me suis rendue compte que j’avais souvent comme des micro-kystes à l’intérieur de la paupière.Cela apparait et disparait mais représente une gène me poussant à me frotter les yeux.
Aussi,j’ai constaté que j’avais souvent des cils qui tombent et se retrouvent dans les yeux et que d’ailleurs, ceux-ci ont tendance parfois à pousser dans le mauvais sens, venant toucher l’oeil (je les enlève à la pince à épiler quand c’est trop genant).
Tous ces facteurs m’ont poussé à me frotter les yeux plus que de raisons…
Par ailleurs, le spécialiste m’a proposé cross-linking + lentille rigite ou cross-linking + anneaux instracorneens.
Je lui ai laissé savoir que je ne souhaitais pas le CXL mais il a l’air de dire que pour je dois d’abord faire le cross-linking pour ensuite avoir les lentilles ou les anneaux.Comme-si en gros je n’avais pas trop le choix.
Il m’a fait comprendre que mon oeil gauche était vraiment atteint et que du coup il fallait préserver l’oeil droit.
Du coup nous devons nous revoir dans 3 mois pour une topographie et pour me laisser réffléchir à tout ça.
Je voudrais juste un suivi de l’evolution de mon kératocone et pourquoi pas essayer les lentilles si ma vue venait à baisser, car pour le moment cela ne représente pas un handicap pour la vie de tous les jours, sauf éventuellement pour la conduite de nuit.
J’ai l’impression qu’on est comme obligé de passer par le CXL dans le cadre du suivi du kératocone, indépendamment presque de notre volonté.J’aimerais trouver un spécialiste qui respecte mon choix sans me mettre la pression en m’expliquant que ma situation est si grave que je ne pourrais me passer de cette opération.
Par ailleurs, j’ai quand même noté qu’il m’a fortement recommandé de ne surtout plus me frotter les yeux et ne plus dormir sur le côté.
En tout cas je vous remercie pour ce site qui m’a beaucoup renseigné et permis de cesser les frottements.
Vous avez effectivement été opérée trop hativement. L’évolution du kératocône n’est pas une fatalité: il faut arrêter les frottements et modifier votre position de sommeil (ne plus exercer de pression contre l’oeil droit pendant le sommeil en dormant sur le ventre ou le côté droit). Le port d’une coque oculaire de protection la nuit permet souvent de protéger l’oeil et au patient de prendre conscience des frottements nocturnes ou du réveil. La pose d’un anneau n’a pas d’effet stabilisateur sur le KC. Les effets sur l’astigmatisme sont parfois un peu imprévisibles. Aussi, les chirurgiens proposent souvent la pose d’un anneau, puis une correction au laser excimer (PKR) associée à un cross linking. La PKR seule est largement suffisante (quand elle est possible, c’est à dire quand la correction n’est pas trop importante) à deux conditions; 1) que la cornée ne soit pas trop amincie par les frottements répétés 2) que les frottements oculaires soient arrêtés en totalité. Vous pouvez donc faire retirer l’anneau s’il vous gêne, vous retrouverez a priori la vision que vous aviez auparavant. Les halos sont probablement liés au bord interne de l’anneau qui est « trop proche » du bord de la pupille. Une surveillance topographique sera nécessaire ensuite, et si vous ne frottez plus, la déformation de votre cornée ne progressera pas.
Bonjour Docteur Gatinel et merci pour vos précieux articles et explications, qui méritent d’être vus par plus de monde encore.
Je vous écrit car je suis depuis quelques mois plongé dans l’anxiété. En septembre dernier j’ai été dans un centre ophtalmo pour un simple bilan, où l’on m’a diagnostiqué un kératocône bilatéral, plus avancé à l’OD et presque dérisoire à l’OG (je précise que je ne porte ni lunettes, ni lentilles). Le chirurgien m’a dit qu’il était urgent d’opérer et que je n’avais pas vraiment le choix, d’abord en effectuant une pose d’anneaux intra-cornéens, puis en complétant ça par du laser excimer + cross linking. Je me suis laissé convaincre car j’ai réalisé ce jour là qu’effectivement, en regardant seulement avec l’OD, je voyais flou, chose dont je ne m’étais jamais rendu compte car les 2 yeux ouverts je n’éprouve aucune difficulté.
J’ai donc reçu l’opération de pose d’anneaux sur l’OD au mois de novembre. Depuis l’opération jusqu’à aujourd’hui, je vois un peu flou alors qu’avant l’opération je n’avais aucun problème les 2 yeux ouverts, et surtout, d’énormes halos lumineux apparaissent maintenant dans mon champ de vision quotidien. J’ai stoppé toutes les procédures car je ne me sentais plus en confiance. J’ai exposé ces gênes à mon chirurgien, qui me répond que tous mes problèmes de vision + halos lumineux devraient se résoudre en continuant les opérations prévues (laser excimer + cross linking).
En lisant plusieurs articles, j’ai le sentiment que cette opération a été précipitée (surtout que le chirurgien a décidé de m’opérer sans avoir de visibilité sur l’évolution de mon kératocône, puisqu’il m’a rencontré une seule fois avant l’opération).
Aujourd’hui je me retrouve avec une vision floue et des halos qui me dérangent jusqu’à en déprimer. Si ces anneaux concernent uniquement la vision et non le ralentissement ou l’arrêt du kératocône, alors je songe fortement à me les faire retirer, mais j’ai peur que mon kératocône évolue et que dans quelques années avoir retirer ces anneaux s’avérerait être une erreur.
Pensez-vous que je puisse m’accorder la sérénité en retirant ces anneaux, sans mettre ma vue en danger pour le futur ?
Il est effectivement utile de contrôler l’évolution, en cas de doute, en réalisant une topographie à un délai plus rapproché (un à trois mois). Le kératocône (et les formes intermédiaire) ne progresse pas/plus une fois l’éviction des frottements oculaires obtenue. Si tel est le cas, alors les contrôles topographiques objectiveront la stabilité de la déformation cornéenne. Idéalement, il faut effectuer des contrôles avec le même instrument, ce qui permet de réaliser une « carte différentielle ». Cette carte est un élément objectif qui permet d’affirmer la stabilité du kératocône (ou, dans le cas contraire, sa progression).
Votre question sur les frottements occasionnés par les manoeuvres de pose et dépose des lentilles de contact sont légitimes. A priori, celles-ci ne sont pas particulièrement dangereuses, car l’intensité de la force exercée contre le tissu cornéen est bien moindre que celle qu’induisent les frottements vigoureux. Les porteurs de lentilles ont souvent tendance à se frotter les yeux après la dépose des lentilles; parfois, ils frottent pendant le port de celles-ci, pour « humidifier » l’oeil (provoquer une sécrétion lacrymale réflexe). Ceci est bien entendu nocif, plus que des gestes plutôt doux et « tangentiels » (sans impact prolongé, et sans les forces de cisaillement générées par les mouvements latéraux ou circulaires qu’effectuent les patients quand ils frottent leurs yeux).
Bonjour Docteur,
J’ai pu comprendre grâce à votre article à quel point les frottements oculaires jouaient un rôle prépondérant dans la venue du kératocône et pouvaient aggraver celui-ci. Après lecture de cet article, je me suis demandé si le geste technique pour mettre et enlever les lentilles pouvait causer une aggravation de la déformation cornéenne en cas de kératocône. En effet , lorsque l’on met des lentilles pour la première fois on est souvent confronté à une multitude d’essais infructueux avant de parvenir à placer correctement la lentille sur l’œil. Le doigt rentre ainsi en contact avec la cornée très souvent même involontairement. Ces contacts avec la cornée s’intensifient lorsque l’on tente de retirer la lentille. Me trouvant moi même confrontée a cette situation j’aurais aimé savoir si ce type de frottements étaient susceptibles d’aggraver le kératocône ou pas. Dans ce cas, serait il préférable dans l’idéal que je ne porte que des lunettes?
Merci a vous.
Bonsoir docteur et merci pour votre réponse. On a ordonné de nouvelles lunettes à mon fils avec une correction plus prononcée. Et une topographie dans 6 mois. Peut on attendre aussi longtemps sans risque ? L’ophtalmologue a un doute de keratocone. Merci beaucoup.
L’orthokératologie peut être une solution à envisager, à condition qu’elle soit efficace dans votre cas (tout dépend du dégré de myopie, d’astigmatisme, etc.). Pour de faibles déformations et des myopies faibles à moyennes, ce type de correction doit être possible. Bien entendu, il est important de ne pas se frotter les yeux au réveil, après retrait des lentilles d’orthokératologie.
Il est effectivement crucial de cesser les frottements oculaires (typiquement réalisés avec les phalanges des doigts chez les patients atteints de kératocône). Dans notre expérience, ceci est nécessaire mais aussi suffisant pour stopper l’évolution du kératocône, ce qui est logique puisque ce sont ces mêmes frottements, exercés généralement depuis quelques années de manière vigoureuse et répétée (plusieurs fois par jour, voire par heure, etc.) qui précèdent et engendrent la déformation cornéenne permanente. Par ailleurs, il faudrait également veiller à modifier une position de sommeil qui serait « sur le ventre », ou « sur le côté », car ce type de position favorise l’irritation oculaire chronique et stimule le besoin de frotter (échauffement local, contamination par les acariens, etc.)
Il faut envisager une greffe pour l’oeil qui a perdu sa vision utile à cause d’un kératocône très évolué. Réaliser une greffe de l’autre oeil (qui voit encore suffisamment) n’est pas indiqué. Pour freiner l’évolution, il est crucial d’arrêter les frottements oculaires. Ceci est souvent difficile à obtenir chez les trisomiques, et c’est pour cela que ces patients présentent souvent des formes graves – car évoluées – de la maladie. Ils se frottent les yeux très vigoureusement et fréquemment, et un cercle vicieux s’installe car l’irritation locale ne fait qu’augmenter. Les frottements nocturnes sont également fréquents. Parfois, le port d’une coque oculaire de protection la nuit peut éviter des frottements sur l’oeil. Bien entendu, il faudra également faire en sorte que les frottements cessent sur l’oeil qui sera greffé.
Bonjour M, j’ai une sœur Trisomique atteinte de la kératocône dans les deux yeux! malheureusement on a pas pu détecter sa maladie jusqu’au jour ou elle a perdu une de ses yeux et il lui faut une greffe de cornée, pour la deuxième œil on nous a dit qu’on doit freiner l’évolution mais ce n’est pas trop urgent, je veux connaître votre avis: est ce qu’on doit commencer par opérer l’œil qui a besoin d’une greffe de cornée, ou bien on commence par celui qui voit encore pour freiner le kératocône…Nous sommes très inquirets dans le contexte d’une trisomie…
Merci Docteur
Bonjour docteur, merci pour vos précieux conseils. Mon fils de 17 ans est hypermétrope depuis tout petit et porte des lunettes. Hier l’ophtalmologue a eu un doute sur le kératocone , il lui prescrit reprit une nouvelle correction et une topographe dans 6 mois, et nous a parlé de lentilles rigides. Ma question : peut on attendre 6 mois sans risque que cela évolue ? qu’en pensez vous? suivant vos conseils je lui ai dit de ne plus se frotter les yeux. Merci pour votre réponse.
Bonjour Docteur,
Les personnes atteintes de kératocône peuvent-elles bénéficier d’orthokératologie ?
Je porte des lentilles rigides en journée que je supporte assez bien, hormis lorsqu’une poussière vient se glisser dans l’œil, c’est-à-dire au moins 10 à 15 fois par jour… Dans ces moments-là porter les lentilles devient une torture, je suis contrainte de les retirer en urgence, ce qui n’est pas toujours possible et parfois dangereux (conduite en voiture par ex.)…
Je vous remercie par avance.
En principe, lors de la découverte d’un kératocône, on commence par essayer d’adapter une paire de lentilles de contact. Si les lentilles corrigent la vision, alors il n’est pas utile de mettre un anneau. En effet, même avec un anneau (dont le but est de réduire l’astigmatisme), il est très probable que l’amélioration de la vision ne sera pas suffisamment marquée pour que vous n’ayez plus besoin de lunettes. A droite, s’il n’est pas possible d’adapter une lentille, alors une greffe peut être la seule solution thérapeutique pour récupérer de la vision. Dans tous les cas, il est crucial que vous cessiez de vous frotter les yeux+++
Bonjour Docteur,
Je viens de consulter le 30/01, et on m’a diagnostiqué un kératocône aux deux yeux avec un stade 3 à l’OG, et un stade 4 à l’OD. Le médecin m’a affirmé que je devais subir la greffe de cornée à l’OD, et m’a programmé d’abord une pose d’anneaux intra-cornéens à l’OG pour le 18/02.
Sachant que je ne vois presque rien avec l’OD contrairement à l’OG que j’utilise principalement, et que je vais commencer un CDI en informatique le 05/03.
Est-ce-que vous pensez que suite à la pose d’anneau je pourrais commencer mon CDI à cette date ?
Merci d’avance de votre réponse,
Bonjour Docteur
je tiens à vous remercier pour votre repense rapide,
en effet j’ai essayé de faire la corrélation entre l’oeil le plus atteint et la position de sommeil, mais je dors souvent sur le coté droit donc normalement c’est l’oeil droite qui devait subir plus de frottement er pression pour mon cas peut être c’est pas la position de sommeil mais plutôt une corrélation entre l’oeil le plus atteint et la sécheresse oculaire. j’ai les yeux secs et l’oeil gauche plus sec que l’oeil droite.
une petite précision pour la vision flou sans correction unilatérale je ne vois pas flou juse avec la correction unilatérale que je vois flou avec les deux yeux et si je ferme mon oeil droite je vois claire avec la correction unilatérale sur l’oeil gauche
Vous avez bien eu raison de cesser les frottements oculaires, cette simple décision suffit pour enrayer l’évolution du kératocône. Les partisans de la réalisation d’un cross linking se gardent souvent de bien expliquer ceci à leurs patients, et ne comprennent pas bien le caractère mécanique de l’affection. Si votre KC était plus avancé sur l’oeil gauche, c’est peut être aussi parce que vous dormez dans une position qui expose préférentiellement cet oeil à une surpression sur le matelas, l’oreiller ou l’avant bras (ex: dormir sur le ventre avec la tête en rotation vers la droite). Il est important de faire attention à cela: là encore, cet aspect est toujours négligé chez les patients alors que la position de sommeil joue un rôle crucial dans la génèse du kératocône (la corrélation entre oeil le plus atteint et la position de sommeil est flagrante: fragilisation par compression, chaleur, et irritation générant probablement une plus grande envie de frotter de ce côté). Je comprends votre crainte vis à vis de l’oeil droit: si vous êtes inconfortable en correction unilatérale, c’est que cet oeil voit légèrement flou (effet du kératocône modéré de ce côté). Il est certain (ou a peu près) que vous ne verrez plus flou après une correction bilatérale. Toutefois, une correction unilatérale n’est pas dangereuse pour les yeux. Ce qui serait dangereux, répétons le, est de poursuivre les frottements oculaires à votre insu.
Bonjour Docteur Gattinel,
Je tiens tout d’abord à vous remercier pour votre site et pour le travail que vous faîte.
j’ai 34 ans et j’ai le keratocone ca fait 8 ans sur les 2 yeux mais beaucoup plus avancé sur l’oeil gauche que la droite, il y a 3 ans j’avais un rendez-vous pour le cross-linking (CXL) a Montréal que j’ai annulé (heureusement) suite a vos suggestions sur ce site 《 j’ai arrêter définitivement de frotter les yeux》 et par la suite j’ai pris la décision d’essayer les lentilles hybride mais juste sur mon oeil gauche ( la plus avancé ) mais adaptation tres difficile (je n’arrive pas a la metre tout seul) correction avec lentilles presque 9/10 mais le problème vu que je mets juste une lentille je vois flous avec les deux yeux et si je ferme l’oeil droit je vois claire (oeil droite sans lentille acuité visuelle 8.5/10 qui a un keratocone qui n’a pas évolué depuis que je ne frotte pas les yeux)
ma question pour cette phénomène de voir flous EST CE QUE si on met juste une lentille c’est normale DE VOIR FLOUS ? le faite de mettre juste une lentille c’est dangereux pour la santé des deux yeux ?
j’ai pris la décision de mettre juste une lentille pour ne pas toucher a la seule oeil qui me reste que grâce à elle je peux vivre sans lentille.
SVP EST CE QUE si je mets des lentilles sur les deux yeux je verrai pas flous ?
MERC BEAUCOUP pour le temps que vous accorder pour nous lir et répondre.
Merci pour votre commentaire; j’approuve tout à fait vos remarques sur les aberrations optiques de la face postérieure de la cornée, « démasquées » par le port d’une lentille rigide. Nous avions étudiés celles -ci dans le passé: http://m1.wyanokecdn.com/ac3f8e3418e778d6b3d582c679483b93.pdf
L’OPD scan III permet de réaliser des simulations de vision à partir d’une image représentant une rue de nuit, je posterai prochainement des exemples sur le site. Je conçois effectivement que le changement de paradigme vis à vis du kératocône que nous essayons de porter devrait beaucoup plus attirer l’attention. Maleureusement, il s’oppose au « business model » en vigueur qui est soutenu par certains acteurs de l’industrie médicale (compagnies qui vendent matériel et consommable pour le cross linking), et ne propose pas d’alternative thérapeutique « payante », puisqu’il ne coûte/rapporte rien de modifier son hygiène oculaire en arrêtant de frotter excessivement ses yeux. La grande majorité du monde ophtalmologique refuse -ou demeure sceptique vis à vis de – ma théorie, ce qui peut être compréhensible après tout, car le scepticisme est une vertu plutôt utile en science et en médecine, et que les idées disruptives mettent du temps à emporter l’adhésion. Ce qui est moins compréhensible, c’est qu’il n’y a pas véritablement d’examen critique de la conjecture « no rub no cone », qui, après tout, pourrait conduire à sa réfutation en bonne et due forme si elle s’avérait érronnée. Il est un peu navrant de constater que conservatisme, intérêts divers, voire une certaine paresse intellecturelle se conjuguent pour continuer à prôner des concepts pourtant démentis par les faits, c’est à dire attribuer au kératocône le label de « pathologie d’origine inconnue, probablement multifactorielle dont génétique », pouvant évoluer spontanément et ne pouvant faire l’objet d’une prévention. J’ai proposé à France 5 de traiter du kératocône à la lumière de nos découvertes, mais il semble que ce thème a été traité récemment… espérons qu’il reviendra prochainement sous les feux de l’actualité! Je continuerai en attendant à communiquer via ce site et defeatkeratoconus.com, en plus des colloques, séminaires et congrès auxquels je participe régulièrement. Les lecteurs qui sont concernés par le kératocône et souhaiteraient porter ces concepts à la connaissance du plus grand nombre sont invités à le faire par le biais de partages sur d’autres sites et réseaux sociaux.
Bonjour docteur je suis suivie par vous depuis 5 ans .
Lors de notre dernier rendez-vous vous m’avez dit que mon Kératocône n’évolue plus car je ne me
Frotte plus les yeux.
Par contre mon astigmatisme a fortement augmenté et ma vue a du coup baisser.
Pensez-vous que les anneaux pourrais m’aider.
Merci
Merci pour votre réponse Docteur. Nous attendons vos publications prochaines avec impatience ! Il apparaît que votre théorie solide vient réconforter énormément les personnes atteintes de KC. Cette pathologie qui vient diminuer drastiquement la qualité de vie, complètement méconnue du grand public, est un supplice. En effet, on vous explique à l’annonce du diagnostic souvent une maladie qui vient inexorablement vous faire perdre la qualité optique des yeux. J’ai eu des ophtalmos nombreux qui parlent seulement en » dixièmes « . J’ai un » stade 3 krumeich » sur l’oeil gauche ( 54 dioptries en kératométrie max ), j’ai 3 dixièmes avec lunettes. Avec des lentilles, 9 dixièmes. L’ophtalmo me dit que cela est satisfaisant, sauf que j’ai du mal à reconnaître les gens ( distorsions visuelles ), une photophobie extrême par rapport à un oeil sain, la vision est pénible voir intenable. Le handicap du kératocône n’est pas dû à la déformation de la face antérieure, car elle peut être régularisée par le port de lentilles, mais c’est la déformation de la face postérieure de la cornée qui est incorrigible et les aberrations sont démasquées par le port de lentilles. Même si la quantité d’aberrations optiques est moindre sur la face postérieure, elle est souvent complètement sous-estimée par les ophtalmos, même spécialistes de cette pathologie. L’opd scan 3 avec les simulations de qualité optique ( images convoluées ) sont un premier pas vers la reconnaissance de ce handicap ( merci à vous ) réel et redoutable. Ma question est la suivante: Pouvez-vous concevoir dans le futur un logiciel avec une prédiction des images du quotidien que peut voir un » kératocônien » , à partir du front d’onde et de la psf ? Cela serait encore plus parlant qu’une planche de lecture, même si c’est déjà super ! Et deuxièmement, vous possédez une information d’une importance essentielle pour le devenir de milliers de personnes pour leur devenir visuel, c’est à dire l’arrêt strict des frottements oculaires stoppe la déformation du KC. Est-il possible, en plus de vos publications nombreuses et sites explicatifs, demander à la chaîne de FRANCE 5 de refaire une émission sur le KC avec vos explications sur le KC ? Cela permettrait une diffusion encore plus large de cette information cruciale ? Nous sommes quand même face à un problème sanitaire majeur, le KC, est de mon point de vue, pas une maladie rare ! Merci beaucoup.
Des publications concernant nos résultats en matière d’étude du lien causal entre frottements et kératocône ont été soumis à publication, ils sont en relecture critique. Quand nos patients cessent de se frotter les yeux (et de dormir avec un appui prolongé sur un oeil ou les deux, donc en levant la possibilité d’une compression et de frottements nocturne), il n’y a pas d’évolution de la déformation, ce qui est assez logique si l’on considère l’étiologie primitivement mécanique de l’affection. Vous pouvez consulter des cas concrets et instructifs sur le site defeatkeratoconus.com . Il n’y a pas de KC héréditaire: ce qui qui est héréditaire, c’est la présence de facteurs de risques pour une déformation accélérée (cornée fine) et pour les frottements (terrain allergique en particulier, milieu favorisant l’irritation oculaire, etc.).
Bonjour docteur je suis suivie par vous depuis 5 ans .
Lors de notre dernier rendez-vous vous m’avez dit que mon Kératocône n’évolue plus car je ne me
Frotte plus les yeux.
Par contre mon astigmatisme a fortement augmenté et ma vue a du coup baisser.
Pensez-vous que les anneaux pourrais m’aider.
Merci
Bonjour Docteur,
Vous parlez de soumettre à publication un nouvel article sur les frottements oculaires. Qu’en pourrons nous le consulter ?
Avez-vous la certitude absolue que l’arrêt des frottements suffit à stabiliser le cône ? C’est très réconfortant pour les malades, mais on a toujours un doute quand on voit que certains kératocônes surviennent très rapidement sans cause apparente. Croyez-vous que cela marche aussi pour les KC « héréditaires » ( oncles, grands mères atteints dans la famille ) ? En tous les cas, c’est très précieux pour nous car l’évolution de la maladie est un supplice pour la plupart des gens atteints.
C’est effectivement une très bonne question et il est crucial de ne pas se frotter les yeux la nuit. Le port de lunettes ou de coques de protection nocturne est un moyen possible pour cela. Mais ce n’est pas toujours très pratique malheureusement…
Bonjour docteur
Comment faire pour dormir autrement que sur le côté je ne me frotte plus les yeux mais il difficilement possible pour moi de dormir autrement je mets des lunettes la nuit pour être sur de ne pas me frotter les yeux pendant del sommeil
Je vous remercie de votre témoignage qui resjoint mes observations. Je ne saisis pas bien en revanche vos reproches concernant la « rétention » d’une information utile. Ce site, ainsi que le site http://www.defeatkeratoconus.com que j’ai créé sont justement dédiés à porter cette information au public. J’ai également publié plusieurs articles (en lien depuis ces sites) sur le sujet et la conjecture « no rub, no cone » (http://beta.jaypeejournals.com/eJournals/ShowText.aspx?ID=14217&Type=FREE&TYP=TOP&IN=&IID=1108&isPDF=YES), qui stipule bien que le kératocône est directement causé par les frottements, et que l’arrêt de ceux-ci en enraye l’évolution. N’hésitez pas à partager les pages de ces sites. La communauté ophtalmologique reste divisée sur ce point, mais un nombre croissant de praticiens réalisent la pertinence de cette théorie, et en vérifie les conséquences positives en notant que chez les patients qui ne se frottent plus les yeux (et modifient leur position de sommeil), le kératocône n’évolue plus. Néanmmoins, comme toujours, un certain conservatisme se heurte à la diffusion de ces concepts, qui entrent également en conflits avec des intérêts financiers (industrie du CXL, honoraires reliés à ces chirurgies, etc). Nous continuons à collecter des données et avons soumis à publication un article scientifique établi à partir d’une étude détaillée des facteurs de risque de kératocône, qui révèle l’influence majeure des frottements et de certaines position de sommeil.
Bonjour Docteur,
Tout d’abord, merci. Merci car grâce à la lecture de votre site, j’ai donc cessé (sans vraiment trop y croire au début) de me frotter les yeux (je ne le faisais pourtant pas beaucoup, mais c’était sans doute déjà trop pour mes cornées). Et verdict avant-hier chez mon ophtalmo : aucune aggravation cornéenne, pas de baisse d’acuité en l’espace de 6 mois alors qu’auparavant c’était la dégringolade perpétuelle…. Et ensuite je vous en veux car j’aurais tellement aimé avoir accès à cette information bien plus tôt. J’en suis -1,75 d’astigmatisme à chaque œil, ça va encore, mais je vis cela comme un handicap, je suis presque dépendante d’une paire de lunettes ou de lentilles rigides… (bon ok il y a pire dans la vie:-) ) J’imagine que vous n’avez pas les pleins pouvoirs pour partager cette information à grande échelle, mais quand même.. détenir une telle information qui peut sauver la vue à de nombreux patients (même si les gens ayant une prédisposition au dvlpt du kératocône sont peu nombreux, ils existent quand même…) et puis s’il faut attendre que la science prouve les observations cliniques des praticiens, je pense qu’on n’a pas fini d’attendre ! Pour ma part, j’informe tous les enfants que je rencontre dans ma pratique (je suis orthophoniste) et je crie au scandale quand j’en vois un se frotter les yeux ! Voyons le positif : me concernant, la stabilité de ma vue est déjà une première victoire…. Mais donc je ne compte pas m’arrêter en si bon chemin : je désire maintenant récupérer une vue parfaite ou presque, de manière non invasive. Le simple fait d’observer le remodelage temporaire de ma cornée suite à un port prolongé des lentilles m’amène à penser que les déformations ne peuvent pas être complètement définitives… Je sais qu’un œil n’est pas un cerveau, mais quand même : parmi mes patients alzheimer avec qui je travaille, j’ai constaté à mon grand étonnement que beaucoup d’entre eux progressent légèrement, pourvu que les stimulations cognitives soient suffisamment ciblées, intensives et vécues positivement par le patient, et cela même à un stade déjà avancé de la maladie ! Donc maladie évolutive/dégénérative ne veut pas forcément dire détérioration inéluctable ou simple stabilité. C’est la plasticité cérébrale qui travaille ok, mais cela peut peut-être se transposer aux cellules de la cornée … ? Je ne connais encore pas grand-chose au fonctionnement de l’oeil, même quasiment rien pour le moment… mais je compte bien apprendre et tenter certaines choses….. Docteur, si vous avez la moindre intuition clinique, information (même surprenante) je suis prête à tenter. Je joue peut-être aux apprentis sorciers mais je me demande, instinctivement, si des massages extrêmement légers, avec les paupières, ou des exercices musculaires répétés chaque jour ne favoriseraient pas une réorganisation des cellules de la cornée ?
Merci par avance.
Bonjour docteur je suis suivie par vous depuis 5 ans .
Lors de notre dernier rendez-vous vous m’avez dit que mon Kératocône n’évolue plus car je ne me
Frotte plus les yeux.
Par contre mon astigmatisme a fortement augmenté et ma vue a du coup baisser.
Pensez-vous que les anneaux pourrais m’aider.
Nous avons effectivement découvert un lien fort entre position de sommeil et kératocône. Si la main est posée sur l’oeil gauche la nuit, il est très probable que l’appui prolongé, l’augmentation de la chaleur locale et les frottements induisent une déformation pérenne de la cornée (c’est à dire un kératocône). Il peut être intéressant de faire porter à votre fils une coque de protection oculaire pour qu’il prenne conscience de frottements et modifie sa position. Plus ici: https://defeatkeratoconus.com/eye-rubbing-tips/
Bonjour Docteur Damien Gatinel , mon fils 20 ans a des problèmes de vision plus prononcés de l’oeil gauche qui me fait penser mais sans certitudes à une keratocone . Quoiqu’il en soit le frottement des yeux savère néfaste.
Il fait attention dans la journée , le problème c’est la position quand il dort . Il dort sur le dos avec la main droite posée directement sur l’oeil gauche .Il y a t-il un moyen pour remédier à cela ?
En vous remerciant , bien cordialement
Un kératocône frustre n’évolue vers une forme plus avérée que si un traumatisme physique local répété (les frottements) est exercé et que ce traumatisme excède la résistance cornéenne. Au delà d’un certain seuil, la réduction de l’élasticité de la cornée peut entrainer une déformation permanente. Dans notre expérience, cette déformation est assez bien corrélée à l’intensité des frottements exercés (même s’il n’est pas facile de quantifier ceux ci, et que les patients se frottent souvent les yeux de manière inconsciente). La position de sommeil est importante et les patients qui présentent un « kératocône frustre » (selon nous une déformation modérée de la cornée, et qui est justement modérée car le stress mécanique cumulé est également modéré) dorment souvent sur le ventre ou le côté (appui oculaire sur l’oreiller, etc.). Les autres troubles visuels que vous rapportez ne sont pas liés au kératocône a priori sauf les images fantômes qui sont la traduction optique de la déformation de la cornée.
Bonjour Dr Gatinel
Un keratocone dit » frustre » qui n’a pas évolué pendant 17 ans peut il evoluer à nouveau ? Un gros stress peut il avoir un impact sur la vision et entraîner de nombreux troubles visuels ( diplopie de pres et de loin ,photophobie , mouches volantes , images fantômes, gêne avec les phares , lumières et soleil ect..) ou bien est ce une évolution des kc..sachant qu’ils n’ont pas évolué d’apres l’ophtalmo et qu’il ne comprend pas ces troubles visuels..
Avec tous mes remerciements
Marie
Le kératocône ne rend pas aveugle, mais peut altérer suffisamment la vision pour handicaper les patients, en particulier quand l’adaptation d’une lentille rigide n’est plus possible, et qu’une greffe de cornée est nécessaire. Ceci ne survient que chez les patients qui se frottent les yeux de manière incoercible. Tout patient atteint de kératocône qui ne se frotte plus les yeux, et qui modifie sa position de sommeil afin de ne pas « appuyer » sur l’oeil (ou les deux) au cours du sommeil ne verra pas la déformation cornéenne progresser. Notre expérience permet aujourd’hui d’établir ce point qui constitue une excellente nouvelle pour les patients atteints de kératocône.
Bonjour docteur
Le keratocone peut il rendre aveugle ?
La force appliquée par le contact de la lentille (appui sur la corné) est minime vis à vis de celle exercée par les frottements oculaires. Un remodelage épithélial peut être engendré par le port prolongé d’une lentille rigide mais cela est transitoire. Il n’y a pas de risque directement lié à la lentille – sauf si l’irritation locale que peuvent provoquer les lentilles déclenche l’envie de frotter les yeux.
Bonjour Docteur,
Je vous remercie pour votre réponse.
Mais êtes-vous certain que les frottements répétés induits par le déplacement de la lentille rigide sur la cornée sont sans danger pour celle-ci, est-ce que cela n’accentue pas le kératocône à long terme ?
Ou peut-être n’avez-vous pas encore suffisamment de recul à long terme pour pouvoir l’affirmer ? Car certes, le port des lentilles rigides donne l’illusion d’une vue presque parfaite retrouvée, mais je ne souhaite pas en payer le prix dans X années… :-/
Je vous remercie par avance. :-)
Merci de votre témoignage très éclairant. Il ne fait aucun doute que les frottements oculaires sont à l’origine (c’est à dire un ingrédient indispensable pour la génèse) du kératocône. Cette théorie sera un jour admise, même si pour diverses raisons, elle n’est pas encore partagée par l’ensemble des ophtalmologistes. Et pourtant, il faut, comme dans votre cas, s’être frotté souvent et vigoureusement les yeux pour déclencher l’apparition d’une déformation cornéenne permanente. Les lentilles rigides sont le meilleur moyen de correction visuelle du kératocône, car elles peuvent corriger des défauts optiques que les lentilles souples (et les lunettes) ne peuvent pas compenser.
Bonjour Docteur Gatinel,
– J’ai 26 ans et ma vue a commencé à baisser progressivement depuis mes 19-20 ans. Alors étudiante, j’étudiais des journées entières et exerçais donc une vue de près de manière prolongée. Le soir lorsque je sortais de mon domicile je voyais extrêmement flou, mais cela était temporaire et après une nuit de sommeil tout allait mieux.
– Mais au fil du temps ma vue a continué à baisser, et cela même en étant moins plongée dans mes livres. J’ai alors consulté. Mais je ne trouvais pas de réponse à mes questions : je ne comprenais pas (n’admettais pas) que ma vue puisse se dégrader à ce point et aussi vite, sans aucune explication. Après un tourisme médical, j’ai rencontré mon ophtalmo actuel, qui elle a pris le temps d’effectuer une vraie anamnèse et m’a expliqué que j’avais peut-être un kératocône : ce fut pour moi la douche froide (je savais déjà ce que cela signifiait suite à des recherches sur internet). Je revois bientôt mon ophtalmo en décembre pour une confirmation/infirmation du diagnostic.
– Ma vue actuellement : oeil droit (-1.75 à 165° ) et oeil gauche -1 (-1.75 à 30°).
– Mon ophtalmo m’a déconseillé de poursuivre mes investigations sur internet, mais la curiosité étant plus forte, je suis tombée assez vite sur votre site internet et ses nombreuses ressources (merci !)
– J’ai commencé à cogiter par rapport aux frottements que vous évoquez comme étant la cause du kératocône : alors je ne sais pas, peut-être que ça m’arrange bien d’avoir cette réponse quant à l’origine de mes difficultés, mais il est vrai en tout cas que les frottements oculaires font partie de mon passé : depuis toujours je me frotte les yeux au matin lors du réveil, le soir lors du coucher et en cas de fatigue en journée (seulement quand je ne suis pas maquillée, c’est-à-dire rarement, ouf). Ces frottements-ci sont assez anodins et pratiqués par de nombreuses personnes sans problème de vue, mais comme vous l’expliquez très bien, de base nous n’avons pas tous la même qualité cornéenne. Depuis l’adolescence j’ai l’impression que la qualité « globale » de mon oeil a diminué : la sclère de mon oeil est plus facilement irritée, rouge (j’ai un passé de conjonctivites persistantes…) et j’ai l’impression qu’elle est fine (on voit des petits vaisseaux, ça n’était pas le cas quand j’étais enfant) mon iris est passé de marron à vert/noisette en grandissant (?). Et depuis toute petite, très curieuse de nature, j’ai expérimenté certaines choses avec mes yeux et notamment des appuis prolongés et intenses sur mes globes oculaires (c’est absurde mais j’étais émerveillée face à toutes les couleurs/effets scintillants que cela provoquait, c’était pour moi un vrai spectacle oculaire :D) En grandissant j’ai arrêté cette plaisanterie et me suis limitée toujours à des appuis intenses, répétés mais en vue de me détendre (à cause de l’anxiété et des insomnies…).
-J’ai une question : étant coquette de nature je ne porte que très peu mes lunettes, mon ophtalmo m’a alors proposé des lentilles RIGIDES. Clairement je ne les supporte pas et j’avoue ne pas persévérer non plus… J’ai peur que cela accentue la détérioration de mes cornées, j’ai l’impression de leur offrir des bouts de verre… Que pensez-vous des lentilles rigides sur une cornée atteinte de kératocône ?
Docteur, je vous remercie d’avoir eu le courage de me lire jusqu’ici.
Je suis ouverte à toute information (je dois encore parcourir plus en détail votre site internet, mais si vous avez de la littérature complémentaire et récente sur le sujet), voire tout essai clinique/expérimentation, bref je suis disponible.
Merci par avance.
Il est difficile sinon impossible de corriger tous les défauts optiques provoqués par le kératocône avec des lentilles souples. Il serait peut être plus indiqué d’essayer d’adapter des lentilles rigides ou hybrides dans votre cas.
Les lentilles souples ne permettent pas de corriger l’intégralité des défauts optiques induits par la déformation cornéenne au cours du kératocône. Il est préférable d’adapter des lentilles rigides (ou semi rigides, ou hybrides) pour réduire significativement ces défauts. L’adaptation de lentilles rigides est la première chose à envisager lorsqu’un kératocône induit une gêne visuelle qu’il n’est pas possible de corriger en lunettes.
Bonjour Docteur,
Je souffre d’un Kératocône. J’ai subis deux opérations à ce jour: un Crossliking d’abord puis une implantation des anneaux Intra-cornées. A la suite de la dernière opération, le chirurgien après deux contrôles m’a prescrit des lentilles de contact souples identiques à chaque œil en terme de paramètres.
Ces lentilles me permettent de voir comme il se doit, c’est à dire la correction du floue, mais je constate depuis déjà quelques semaines qu’elles ne sont pas trop adaptées car actuellement, j’ai comme un floue sur les images que je fixe ou encore les écritures.
De ce fait, je voudrais savoir svp, s’il est possible refaire (chez un autre ophtalmo spécialisé en lentilles de contact souple) des examens approfondis et contrôles afin de bien vérifier ce qui ne va pas mais aussi qu’au sortir de là me prescrire des bonnes lentilles de contact souples svp, c’est-à-dire qu’il puisse m’adapter ou me prescrire des lentilles de contact souples adaptées à la correction voulu selon les résultats d’analyses trouverées?
Je vous remercie d’avance pour votre retour de réponse et l’attention que vous porterez à ma demande.
C’est un point délicat dans l’adaptation et le port de lentilles rigides: la survenue d’une conjonctivite giganto papillaire doit faire revoir les modalités de l’adaptation contactologique (type de lentille, de produit, etc.). Il faut en discuter avec votre contactologue qui maitrise ces paramètres et dispose de donnnées d’examens spécifiques comme la position et le comportement de la lentille sur la cornée, etc.
Bonjour Docteur,
J’ai 34 ans et je souffre d’un Keratocone Bl latéral évolutif stade 3, 4. Je portais des lentilles rigides de type Eyebride de LCS en piggyback. Vision 10/10 et pas de lunette possible.
Depuis 6 mois, j’ai une conjonctivite Gigapapilaire, ça me donne des douleurs aux yeux avec et sans lentilles, douleurs qui remonte dans les tempes.
On m’a conseillé de changer de matériaux de lentilles. Je suis en adaptation avec dès sclérales toujours de chez LCS. Adaptation difficile, ça me donne des vertiges et maux de têtes.. + temps de ports peut convenable autour de 7h. Quand pensez vous? Comment soigner cette conjonctivite Giga papillaire en continuant à porter des lentilles ?
Merci
Au vu de votre correction, la déformation cornéenne doit être assez mineure, car sinon vous auriez un astigmatisme beaucoup plus prononcé. Cessez de frottez vigoureusement vos yeux, et les choses ne devraient pas beaucoup évouluer. Il peut s’agir d’un diagnostic de kératocône posé par excès; prenez un autre avis.
Bonjour,
J’ai 33 ans et j’ai un kératocone détecté octobre 2017 mais le spécialiste m’a dit qu’il ne fallait rien faire car j’avais un bon visuelle oeil gauche : -0.5 (-0.75), oeil droit 0.75 (-0.50) … et j’ai refait un test à ce jour aout 2018 : oeil gauche : -0.75 (-0.50), oeil droit 0.50 (0.50) … est ce possible que j’ai pu améliorer ma vision légèrement ? et la perte de l’oeil gauche est elle inquiétante selon vous ? je vois légèrement plus flou une petite gêne (sachant que je suis très anxieux je ne pense qu’à cet oeil …) et quand ça gratte, je touche légèrement les côtés de l’oeil et les cils ( est- ce bon ou mauvais ?) … et les lunettes sont ils nécessaires sachant que je passe 8h devant un ordinateur et portable et que ça doit fatigué l’oeil ? Merci de votre réponse et votre attention …
Merci beaucoup docteur de votre reponse
Bien cordialement
Les anomalies (aberrations) optiques induites par le kératocône ne sont pas corrigibles en totalité avec les verres de lunettes. De plus, la correction de l’astigmatisme (souvent prononcé) des patients atteints de kératocône occasionne des troubles liés aux aberrations ou distorsions qui peuvent être induite par les verres de lunettes qui portent une forte correction de l’astigmatisme. Il est plausible que votre cerveau s’adapte à un type de correction, en trouvant un compromis, et que les changements de correction ultérieurs déstabilisent cette adaptation. En tout état de cause, il est certainement utile que vous tentiez une adaptation en lentilles de contact. Les lentilles sont le meilleur moyen de correction des aberrations optiques provoquées par le kératocône. Plus d’informations sur les anomalies visuelles observées dans le kératocône (en anglais) : https://defeatkeratoconus.com/vision-disturbances-of-keratoconus/
Bonjour docteur.
J’espère que vous prendrez le temps de me lire….
J’ai un keratocone modéré, mon ophtalmo ne souhaite pas m’équiper en lentilles , car il est « modéré » même si ce terme ne veut rien dire pour moi car mes galères ne le sont pas…..
Quand je change de lunettes je ne les supporte pas ( inconfort, maux de têtes etc…) je ne supporte plus que ma vieille paire de lunettes ou alors je dois racheter toujours le même type de lunettes ( percées, petit verres même marque) et encore…..
Je trouve cela etonnant , je suis suppose que le keratocone en est la cause.
Je précise qu’ il a été découvert par hasard il Ya 3 ans, car de guerre lasse avec ces problèmes de lunettes, j’ai souhaité me faire opérer.
Je porte des lunettes depuis l’âge de 16 ans , j’en ai 43, j’ai commencé par etre myope puis l’astigmatisme est arrivé vers 30 ans ….et les galères de lunettes ont alors commencé ….
J ai essaye de porter d autres sortes de lunettes, verres plus grands en acétate, plus près des yeux aussi…
C est comme si mes yeux ( mon cerveau) en se déformant jour après jour , « enregistrait » les caractéristiques des verres, leur géométrie, puis lors du changement de lunettes ( meme à correctionsmeme égales)n’en voulait plus d’autres.
J’ai lu des tas d’articles sur le keratocone, tres peu parlent de l’inconfort mais plutôt d’une mauvaise vision.
Je précise que l’orque j’étais plus jeune je changeais de lunettes tres facilement plus ca s’est dégradé avec les années…
Dois arrêter les lunettes, m équiper en lentilles je suis perdue ( nb j ai fais des tas de séances d’orthoptie qui n’ont rien changé)
Merci d’avance
Cordialement
Myriam Gonzalez
Il convient de vérifier qu’il s’agit bien d’un kératocône car la réalisation d’une topographie cornéenne est parfois difficile chez les enfants en bas age, et qu’il s’agit d’un âge très précoce pour développer cette affection. Si votre fille s’est frotté les yeux de manière acharnée depuis qu’elle est en age de le faire, ceci pourrait corroborrer ce diagonstic. Néanmoins, il s’agit probablement d’un diagnostic posé par excès. Refaites la topographie, et surtout, veillez à ce que votre fille ne se frotte pas les yeux, notamment avec les poings et les phalanges.
Bonjour docteur,
je viens d’apprendre que ma fille agé de 4 ans a un keratocone. Son medecin ma demandè de faire le topo chaque 3mois, et avoir des lunettes. Est ce qu’il ya d’autres solutions pour le stopper !!!
Il existe effectivement une étroite corrélation entre vision et topographie: les symptômes visuels ressentis par les patients atteints de kératocône sont induits par la déformation de la cornée (astigmatisme irregulier qui n’est pas corrigible en lunettes). Les patients atteints de kératocône peuvent toutefois ressentir certaines fluctuations de leur vision, en fonction de l’éclairage ambiant, l’état de la surface oculaire, etc.
La déformation cornéenne, qui est en fait la réelle entité du kératocône, est celle du stroma. L’épithélium est une couche assez fine (10 pc de l’épaisseur cornéenne totale environ). Le kératocône est provoqué par un stress mécanique répété (les frottements) qui est transmis à toute la paroi cornéenne. Il n’est pas inhabituel que des divergences existent pour juger de l’évolution d’un KC, car les cartes topographiques sont moins répétables dans le cadre du KC que chez des sujets normaux. Ce qui est certain, c’est que si vous ne frottez plus vos yeux, les chances de progression sont nulles. Le KC n’est pas une maladie génétique qui évolue pour son propre compte, mais une déformation primitivement mécanique.
Les lentilles ne sont en rien délétères pour le kératocône. Au contraire, les lentilles rigides (ou hybrides) constituent, et de loin, le meilleur moyen de correction pour le kératocône. Les anneaux intra cornéens sont loins d’apporter le même bénéfice visuel. Le cross linking est parfois source d’une aggravation de la vision dans les premières semaines postopératoires, et, commen expliqué sur ce site, ne sert pas à grand chose si ce n’est à donner l’illusion d’une prise en charge thérapeutique. En revanche, il est crucial de ne pas frotter ses yeux lors du retrait des lentilles, ou au cours du port de celles ci.
Bonjour docteur Gatinel,
J’ai 30 ans et Je souffre d’un kératocône non évolutif au deuxième stade sur l’œil droite. De ce fait les lunettes ne me suffisent pas. J’envisagerai donc de porter des lentilles. Mais j’ai une question, est ce que le fait de poser et enlever les lentilles ne causera pas de problème sur le long terme ?Puisque c’est un contact direct avec l’œil.
Merci d’avance.
Bonjour,
Pour ma part arrêter de me frotter les yeux m’est devenu possible quand j’ai pu diminuer drastiquement les moisissures dans mon appartement.
J’ai une question au Dr Gatinel, comment est-ce possible qu’une irritation superficielle des yeux puisse avoir un impact sur le stroma ?
En somme un frottement des yeux ne devrait pas avoir d’impact sur le devenir du kératocone, puisque c’est bien la couche profonde qui entre en jeu.
C’est une question qui me semble importante car on m’a dit que mon kératocone s’était aggravé, puis un autre avis « un peu » aggravé, en substance je n’ai pas l’impression que ça s’est tellement aggravé au final.
D’autant plus que pour faire un Cross Linking, on gratte carrément l’épithélium qu’on enlève complètement, si vraiment une irritation superficielle aggraverait le kératocone on ne ferait pas de Cross linking.
Bonjour,
J’ai 49 ans et j’ai un keratocone bi lateral, diagnostiqué depuis l’age de 20 ans. Je porte des lentilles rigides depuis et le keratocone n’a pas evolué, et la vision reste stable avec les lentilles. Ma uestion est la suivante: Y-a-t-il une correlation entre la vision et la topographie ? En d’autres termes, si ma vision bouge, c’est à dire que la cornée à bougé également, donc il faut refaire une topographie. Je ne m’étais pas posé la question car ma vision ne bouge pas…
Il est effectivement très important de ne plus vous frotter les yeux. Le faire avec la pulpe est certainement moins délétère qu’avec les phalanges. Cette page fournit de nombreuses recommandations pour ne plus se frotter les yeux: https://defeatkeratoconus.com/eye-rubbing-tips/
Le dédoublement des lettres et des textes imprimés est lié à de l’astigmatisme, dont une composante est régulière (corrigible en lunettes), et l’autre dite « irrégulière » (non corrigible en lunettes). Le port de lentilles rigides permet souvent d’atténuer ces symptômes.
Plus sur la vision des patients atteints de kératocône:
https://defeatkeratoconus.com/vision-disturbances-of-keratoconus/
Il est parfois possible d’améliorer au moins partiellement la vision avec des lunettes. Le plus important, pour éviter que le kératocône progresse, est de ne plus vous frotter les yeux.
En ce qui concerne votre oeil gauche, il est probable que la solution réside en une greffe de cornée, si celle-ci présente des opacités et ne peut plus recevoir de lentille. Pour l’oeil droit, la pose d’anneaux peut effectivement être envisagée, mais les résultats sont souvent inconstants: si votre oeil est myope, il faudra porter des lunettes ou une lentille malgré la pose d’anneaux. Or, les anneaux compliquent parfois l’adaptation secondaire d’une lentille de contact…
Bonjour docteur Gatinel,
On m’a détecté un kératocône évolutif en 2010 sur les 2 yeux. J’ai eu un cross linking de l’oeil gauche en 2011 et de l’oeil droit en 2012. En 2013 j’ai été équipe en lentilles rigides que j’ai très mal supportées, du coup l’adaptatrice m’a mis des lentilles Hybrides. Mon kératocône a continué d’évoluer, et en décembre 2017 j’ai eu une kératite amibienne à l’oeil gauche et du coup mon oeil est plus sensible. A la fondation Rothschild on m’a fait des topographie qui montre que ma cornée est trop fine à gauche du coup impossible de poser des anneaux intra-cornéen, mais à la droite il est encore possible.
quelles sont les avantages d’une pose d’anneaux intra-cornéen?
quelle serait la solution pour mon oeil gauche très affecté?
Quelle solution pour mon cas?
On me parle de greffe de cornée mais j’ai très peur car je suis très jeune je n’ai que 29ans?
J’ai peur de cette intervention
Merci de toute r
Bonjour. J’ai également un keracotone.
On me fait porter actuellement des lentilles. Mais je souhaiterais savoir s’il serait possible de gagner en acuité visuelle quand je ne porte pas mes lentilles.
Mon travail pourrait me virer si ma vue baisse…
Bonjour, je suis ici car j’ai été diagnostiqué d’un kératocône mi-avril. Je constatais des troubles de la vision depuis pas mal d’années, et ceux-ci s’étaient accentués rapidement ces derniers mois. J’ai 34 ans.
L’ophtalmo a donc diagnostiqué un kératocône et m’a très fortement conseillé de ne plus jamais me frotter les yeux et m’a prescrit une paire de lunettes (je n’avais jamais porté ni lunettes ni lentilles jusqu’alors).
Depuis, j’ai essayé d’arrêter de me frotter les yeux, et ai constaté que je me frottais les yeux souvent, sans m’en rendre compte. Mes yeux me piquent souvent et j’ai beaucoup de mal à m’empêcher de me les frotter : je le fais donc dorénavant doucement, sans appuyer, et en utilisant uniquement les « pulpes » des doigts (là où se trouvent les empreintes) plutôt que les phalanges : est-ce suffisant ? Dans le cas contraire, comment pourrais-je freiner cette envie incessante de me frotter les yeux ?
Autre question : avant ce diagnostic, je savais que ma vision était à corriger, mais je n’imaginais pas un cas comme celui-là. Mais depuis ce diagnostic, j’ai l’impression que la gêne a subitement augmenté, sans parvenir à déterminer si cela est réel, ou psychologique. Je vais avoir mes lunettes en fin de semaine, je sais déjà que cette correction ne sera pas optimale mais je crains qu’elle ne soit même pas efficace. Et j’ai du mal à comprendre quelle correction est à privilégier pour un cas comme le mien : j’ai lu que les lunettes ne suffisaient souvent pas, que les lentilles n’arrangeaient rien, que le cross linking était inefficace et que la chirurgie était à réserver aux cas les plus graves…
En fait, ma question est simple : quand je lis un texte, je vois les lignes en double : est-ce que cela peut se corriger (et si oui : comment) ou est-ce irrémédiable (et le cas échéant : que dois-je faire pour que ma vision soit la moins mauvais possible) ?
Merci beaucoup.
Il n’est pas nécessaire de porter des lentilles rigides si vous êtes relaitvement à l’aise sans correction. Vous pouvez porter des lunettes occasionnellement (ex: conduite, spectacles, etc.). Le plus important, comme vous l’avez compris et réalisé, est de ne plus vous frotter les yeux: votre déformation ne progressera plus si vous cessez définitivement de malaxer vos cornées!
Je vous conseille de consulter le site de l’association française du kératocône, qui devrait, j’espère pouvoir vous orienter: http://www.keratocone.net/presentation.html
Bien souvent, les contrôles topographiques réalisés dans ce contexte ne sont pas « fiables » (il existe une grande variabilité d’un examen à l’autre pouvant laisser penser à une progression, alors qu’en réalité il s’agit d’un biais de mesure). S’il n’y a pas de perte d’acuité, cela veut dire en tous les cas que la situation n’est pas alarmante; Refaite un (voir plusieurs) contrôles topographiques, si possible avec la même macbine qu’initialement. Il est important bien entendu de vérifier que vous avez cessé de vous frotter les yeux (à votre insu?).
Bonjour Docteur,
J’ai un Kératocône bilatéral diagnostiqué à l’âge de 27 ans, j’en ai actuellement 39. J’ai été opérée avec plusieurs années d’intervalles d’anneaux intra-cornéens sur mes deux yeux. J’ai dernièrement fait une topographie de contrôle et il s’avère qu’il y a une reprise de la maladie sur mon œil droit mais pas de perte d’acuité visuelle. Je ne vous cache pas que je suis inquiète. Faudra-t-il songer à retirer mon implant ? Songer à une greffe ?
Bonjour Docteur,
Mon kératocône oeil gauche a été diagnostiqué il y a 1 an et demi (j’ai 32 ans). Des lentilles rigides m’ont été prescrites mais l’adaptation a été faite certainement trop rapidement et je ne les ai jamais supportées. AUjourd’hui j’ai changé d’ophtalmologue, et il se trouve que mon kératocône oeil gauche a évolué en stade 4 (j’ai moins d’1/10), et que le droit a évolué également (j’ai moins de 5/10). J’ai rdv avec un spécialiste courant juin pour discuter d’une éventuelle greffe pour l’oeil gauche. En attendant, j’ai repris une adaptation lentille rigide sur l’oeil droit.
Enseignante, je suis contrainte d’exercer à 120 km de mon domicile et mon administration, ne connaissant pas la maladie comme bon nombre de personnes, ne la prend pas au sérieux et refuse de me muter pour ce motif. La MDPH de mon département refuse également de m’octroyer le statut de travailleur handicapé, pour appuyer ma demande de mutation.
J’ai donc demandé de nouveaux certificats médicaux, mais
Existe-t-il une brochure, ou tout autre support, à destination des médecins des administrations, afin de leur faire connaître la maladie et surtout ses conséquences sur notre vie quotidienne et ainsi, pouvoir leur faire prendre la mesure de ce que cela implique et les « contraindre » à adapter nos postes de travail?
Bjr docteur,
J’ai 27 ans et Ils m’ont diagnostiqué un KC stade 2 d’aprs mon docteur et stade 1 selon mon ophtalmo …
mon ophtalmo Ma conseillé des lentilles rigide mais le prob c’est que mes yeux produise un peut de larme est ça gene et fause le resultat de la Correction .. je suis un peut perdu
PS : ma vu actuellement ODG 7/10.. mnt J’hésite a prédre ces lentilles
Ma qustion esque Je peux rester sans lentilles ? Et vivre normalement , j’ai arreté de Frotter mes yeux ,Ça m’arrive de frotter sur les bordures
Merci pr votre rep Dr
Merci pour vos précisions.
Concernant le PKR, je reviendrais vers vous par mail dans un premier temps.
Je possède des topographies annuelles (ou presque) concernant les évolutions de ma cornée.
Donc si c’est quelque chose d’envisageable, je serais preneur.
Aujourd’hui, je possède toujours un terrain allergique, donc je fais fasse régulièrement à des envies de frotter, et forcément je ne cède pas. Je suis donc convaincu face à cela.
Votre témoignage est malheureusement le reflet de pratiques médicales que l’on peut juger négativement. Il n’y a jamais d’urgence à réaliser un CXL, et l’intérêt de cette technique (pour le patient éclairé qui est capable de contrôler ses frottements) n’est pas justifié quand les frottements cessent. C’est ce dont votre oeil gauche (comme ceux de tous les patients que je suis pour KC) témoigne. Le KC est provoqué par les frottements (sans frottements, pas de kératocône), et il est également (par le biais des frotteements) très lié à une position de sommeil particulière comme l’appui profond de la tête dans l’oreiller (position de côté ou sur le ventre). Comme vous le mentionnez, les OPHs qui réfutent la responsabilité directe d’un traumatisme dans la génèse du KC sont bien en peine de trouver une autre explication. Les frottements ne constituent pas une explication par défaut du kératocône, car il existe un lien direct entre côté le plus frotté et l’oeil le plus atteint, et par ailleurs, les frottements précèdent l’installation du KC de quelques années en général. Ils agissent comme un agent « vulnérant ». On peut faire une analogie avec la cause des coups de soleil (érythème solaire). Ils sont liés à une exposition trop forte aux UV, comme la cornée l’est aux frottements chez certains patients. Pas d’UV, pas de brulûre, pas de frottements, pas de lésion traumatique.
Si vous êtes absolument certain de ne plus frotter, une opération par PKR est tout à fait possible sur l’oeil faiblement déformé (laser de surface). J’en ai l’expérience sur votre terrain.
Bonjour Docteur,
Merci pour cette rédaction permettant de (je trouve) répondre efficacement au kératocône.
Diagnostiqué en 2013 (âgé de 22 ans), d’un kératocône à l’oeil droit, on me propose une opération, le lendemain …
Je décide d’attendre un contre avis, qui sera le même, KC sur oeil droit, on me propose donc dans l’immédiat un Cross Linking.
On me diagnostique quelques temps après le KC sur l’oeil gauche.
J’ai depuis stoppé tout frottement sur les yeux, cela peut m’arriver, mais c’est très rare, et uniquement en bordure et délicatement.
Je suis à ce jour avec une évolution plus que minime sur mes deux yeux. Alors que seul l’oeil droit a été opéré.
Pour ma part, je possède un terrain allergique avec essentiellement rhinite allergique en début de printemps.
Je confirme votre rédaction, les frottements sont très probablement LA CAUSE du kératocône.
Aucun docteur rencontré n’a pu m’expliquer clairement le kératocône …
En dehors de cela, je voulais savoir étant donné mon astigmatisme et une faible myopie, est-il possible d’envisager une opération de correction visuelle sur un patient atteint d’un léger KC avec une épaisseur cornéenne satisfaisante ?
Bien à vous,
Et bonne continuation pour cet article et vos recherches
Concernant le kératocône de votre fils, il est crucial que les frottements cessent définitivement. Comme expliqué sur ces pages, les frottements sont l’ingrédient nécessaire pour l’apparition d’un kératocône, et ceux que vous décrivez sont les plus fréquemment incriminés chez les patients atteints de KC (car ils sont vigoureux et effectués avec la partie « dure » des doigts et des mains). De mon point de vue, le CXL n’a pas d’intérêt chez les patients atteints de KC (sauf s’il induit de part l’inflammation provoquée localement l’impossibilité pour le patient de continuer à frotter). En effet, contrairemnt à l’assomption qui considère que le KC est le fruit d’un ramollissement tissulaire spontané, cette maladie est en fait le résultat d’un traumatisme local répété. La suppresion de ce traumatisme suffit à stabiliser tous les KC que je suis, et ces cas, anonymisés, sont consultables ici. Je consulte régulièrement pour le KC, en particulier son dépistage et prise en charge précoce à la Fondation Rothschild, à Paris.
A priori, il n’existe pas de prise en charge spécifique concernant le travail sur écran chez les patients atteints de kératocône. Le travail prolongé sur écran est certainement éprouvant pour les patients dont la vision est réduite, et par ailleurs, nous avons observé qu’il était un facteur de risque pour les frottements oculaires. Il est important de résister à l’envie de frotter, et aménager si possible l’ergonomie de votre poste de travail.
Docteur,
Je me permets de vous contacter car j’ai un keratocone bilatéral. Dépistée dans les années 90, j’ai subi une greffe de cornée à St Etienne en 2002 sur l’oeil gauche.
J’ai de l’eczéma depuis toute petite et me frotte très régulièrement les yeux. J’ai une sècheresse oculaire certaine. Cependant, lorsque j’instille des larmes artificielles, j’ai encore plus envie de me frotter les yeux.
Actuellement équipée en lentilles SPOT.
J’ai en plus de mes lentilles depuis septembre 2017 une paire de lunette supplémentaire pour soit disant travailler. Cependant, je ne peux plus m’en passer.
A ce jour, je travaille plus de 39h/semaine sur un écran d’ordinateur. J’ai des douleurs de plus en plus derrière le globe occulaire et des maux de tête.
Je songe à réduire mon temps de travail (pour réduire le temps sur écran).
Savez-vous si les patients atteints de cette maladie ont droit à une quelconque prise en charge pour une réduction de temps de travail liée à cette pathologie ?
Je vous remercie de vos informations.
Cordialement,
Bonjour Docteur,
Mon fils de 17 ans a été diagnostiqué d’un kératocône stade 2 sur l’oeil droit et stade 1 sur l’oeil gauche, le 7 février dernier. L’ophtalmo lui a prescrit des lunettes pour corriger l’astigmatisme de l’oeil droit mais il est magré tout gêné, surtout la nuit et lorsqu’il conduit (conduite accompagnée) : traînées, dédoublements, etc…Une visite de contrôle est prévue en juin pour évaluer l’évolution, après arrêt des frottements (notre ophtalmo y est sensibilisé). Ceux-ci sont avérés, très fréquents, surtout du côté droit, sous forme de malaxage des yeux avec la base du poignet (yeux qui grattent, contexte allergique). Si il y a évolution en juin (PENTACAM), il sera proposé un cross-linking. Nous sommes très perturbés par l’annonce de ce kératocône, qui intervient à un âge ou l’avenir se construit. Nous sommes prêts à prendre plusieurs avis et en particulier à venir vous consulter sur Paris car intéressés par votre approche (nous consultons aujourd’hui sur Vannes). Quelles seraient vos recommandations de façon à prendre en charge ce problème de la meilleure façon qu’il soit.
Vous remerciant.
Il serait utile de connaître le type d’intervention réalisé sur votre oeil gauche. Il est possible que vous souffriez d’une hypersensibilité cornéenne, mais cela reste à confirmer. Le fait que vous « sentiez » la cornée lors des mouvements oculaires (frottement contre la paupière) accrédite cette hypothèse.
D’importants progrès ont été réalisés en contactologie, avec la mise au point de nouvelles générations de lentilles sclérales et hybrides (rigides au centre, souples en périphérie). Il est important de consulter un contactologue spécialisé dans l’adaptation du kératocône et des greffes. Et, last but not least, il serait nettement préférable que vous cessiez de vous frottez les yeux. Ceci peut avoir un retentissement certain sur les cornées et les greffes.
Bonjour j’ai 66 ans j’ai subi 2 keratoplasties des 2 yeux en 1975 et 1995. Je me frotte énormément les yeux et je ne peux pas m’en empêcher. On a essayé en 1995 de m’équiper de lentilles toriques mais le greffon décentré frottait sur la lentille. Des progrès ont ils été réalisés qui me permettraient d’améliorer ma vision qui est nettement moins bonne avec des lunettes
J’ai porté des lentilles dures puis des verres scleraux avant la première opération
Si vous pouviez m’annoncer une possibilité d’équipement avec une nouvelle technologie ce serait épatant
Merci pour toutes vos informations
Bonjour docteur.
Alexandre 24 ans.
Sujet à une sécheresse oculaire sévère (Blepharite + dermato conjonctivite atopique chronique) et à un Kerato bien évolué OG, je me suis fait opérer à cet oeil en octobre 2016. Ce kérato n’aurait pas beaucoup évolué depuis (Je fais de mon mieux pour ne pas me frotter les yeux..)
Je me permets de vous écrire car cela fait maintenant 7 ans que je suis sujet à des douleurs, surtout au niveau de l’œil gauche, où Le Keratocone est le plus évolué.
Ces douleurs sont insupportables, je suis allé voir des centres opthtalmos et suis même monté aux 15-20 à Paris.. PERSONNE ne me donne la moindre réponse.
Ces douleurs se traduisent ainsi : douleur généralisée au niveau du globe, et rapidement grosses céphalées. Une sensation de migraine énorme « dans » l’œil, et ensuite sur tout le front.. Et c’est comme ci je sentais la cornée, suite aux mouvements des yeux (Sentir le bout de l’oeil toucher la paupière.. pas évident d’expliquer par message!)
Je suis sous tramadol LP 50 voir 100 car ma vie personnelle et professionnelle sont énormément touchées par tout ça.
J’ai des gouttes, de La vitamine A, et je suis en train d’essayer mes premières lentilles rigides, pour le moment je ne Les supporte pas du tout.
Je me demandais si vous pouviez me conseiller pour ces douleurs invalidantes, qui me font passer pour un fou auprès des dits spécialistes..
J’ai fait une IRM, j’ai même vu un neurologue… Mais ces douleurs sont bien présentes, non crées par mon système nerveux.. pas de doute là dessus.
Après des années de recherche si je puis dire, ma seule explication serait une fatigue visuelle très importante, et un terrain allergique qui empirerait tout cela.. Mais ce n’est que mon avis de patient.
Je suis à bout de solution.
Merci de votre site, de votre point vue rationnel, descriptif et très aidant concernant le Kerato.
Merci pour une éventuelle réponse.
Respectueusement,
Alexandre
Il n’est pas possible de guérir du kératocône, mais il est tout à fait possible de stabiliser son évolution en arrêtant définitivement de se frotter vigoureusement les yeux. Le kératocône n’est pas une maladie héréditaire, mais la conséquences d’un terrain propice aux frottements, c’est à dire généralement atopique (allergies), avec fatigue, stress (les yeux sont fatigués et donnent envie de les frotter, etc.). La position de sommeil est un élément important; les patients qui dorment sur un côté (la tête appuyée dans l’oreiller) on souvent un kératocône de ce côté (ou plus marqué du côté le plus « appuyé » pendant la nuit. Si, avant la survenue de frottements répétés et prolongés dans le temps, la cornée est fine, le kératocône (la déformation permanente de la cornée) surviendra plus rapidement.
La sécurité sociale rembourse les collyres (anti allergiques, hydratants) et certaines opérations liées au kératocône. Les lentilles sont en général l’objet d’une prise en charge dans ce contexte, et constituent le moyen de correction visuelle le plus efficace.
Les dernières avancées dans cette maladie sont de mon point de vue le fait qu’elle peut être prévenue et stabilisée si l’on accepte l’hypothèse d’une origine directement liée au frottements (pas de frottements, pas de kératocône, « no rub, no cone »). De nombreux éléments logiques, et d’innombrables observations cliniques bien conduites soutiennent cette hypothèse. Elle ne fait malheureusement pas l’objet de beaucoup d’intérêt de la part de ceux qui préfèrent prescrire des techniques coûteuses (et inefficaces quand au premier but recherché, durcir la cornée), comme le cross linking (CXL). Il n’est pas tant important de (tenter de) durcir une cornée ramollie par des années de frottements répétés que de cesser ces frottements! Un site est consacré au kératocône (en anglais): https://defeatkeratoconus.com/ Il rassemble tous les cas vus depuis cette dernière année et suivis depuis plusieurs années par mes soins pour certains. Tous sont stables: car tous les patients ont arrêté de se frotter les yeux, et évitent de dormir sur le ventre ou le côté (ce qui est très corrélé au kératocône).
Bonjour Docteur et merci pour ce que vous faîtes.
J’aurais deux questions à vous poser.
La première, est-il possible de guérir du kératocône ?
La seconde, y a t’il une évolution pour la prise en charge de la Sécurité sociale ?
Quelles sont les dernières avancées concernant cette maladie ?
Merci d’avance !
Signé, un patient qui ne supporte pas ses lentilles rigides…
Merci pour votre témoignage. L’arrêt de la progression de votre kératocône ne tient pas du miracle ;-)
Le kératocône est induit par les frottements répétés et particulièrement soutenus des yeux; en l’absence de frottements (ou à l’arrêt de ceux-ci), il n’y a pas de progression. Cette découverte, que nous avons illustrée par l’exemple ( voir les cas rassemblés ici: https://defeatkeratoconus.com/portfolio-filtersearch/ et qui ne sont pas triés), ne fait pas l’affaire des adeptes du CXL. Néanmoins, tout patient découvert avec un kératocône devrait recevoir une information étayée sur les frottements, être invité à prendre conscience de frottements oculaires intempestifs, et suivi avec des cartes topographiques différentielles… qui révèlent à chaque fois l’arrêt de la progression quand les frottements s’arrêtent.
Concernant vos questions relatives à des symptômes visuels:
1) les halos visuels sont en grande partie la conséquence de la déformation cornéenne. Cette déformation est responsable d’une réduction de la qualité optique de l’oeil: la perception d’un écho autour des lumières vives (ex : plusieurs croissants de lune dans le ciel la nuit), de halos, de dédoublement des images constrastées (ex; sous titres) découle de l’asymétrie de la cornée (qui est la lentille optique la plus importante de l’oeil). Pour y remédier, le meilleur mode de correction consiste en l’adaptation de lentilles rigides. De nombreux progrès ont été accompli dans la réalisation des lentilles pour l’équipement des cornées atteintes de kératocône (lentilles hybrides en particulier, qui conjuguent le confort des lentilles souples et la qualité de correction des lentilles rigides). Cette page est un peu technique mais essaye d’expliciter l’effet des aberrations optiques impliquées dans la distorsion visuelle des patients atteints de kératocône; https://defeatkeratoconus.com/vision-disturbances-of-keratoconus/
2) Il n’y a en revanche pas de traitement pour les corps flottants usuels, qui sont liés à la myopie, et peuvent être plus facilement perçus quand on regarde un motif uni comme un mur blanc, le ciel, etc.
Bonsoir Docteur Gattinel,
Je tiens tout d’abord à vous remercier pour votre site.
J’ai 30 ans, je souffre d’une forte myopie depuis mon jeune age et j’ai été diagnostiqué d’un kératocône bilatéral en 2013 au CHU d’Antibes, kératocône qui a évolué rapidement et fin 2015 on m’a proposé un CXL dans un cabinet externe (moyennant 800 Euros). C’est à ce moment où j’ai découvert votre site. J’ai essayé de ne plus me frotter les yeux depuis, et miracle ! le kératocône n’a quasiment plus évolué. Si jamais j’aurai eu cette recommandation avant, ça m’aurait évité cette dégradation.
Aujourd’hui j’arrive encore avec les lunettes à avoir 10/10 car la déformation est décentrée sur mon oeil gauche, par contre mon oeil droit avec la correction atteint 5/10 maximum car la déformation est centrée.
Je voulais prendre votre avis sur deux phénomènes qui me gênent et qui je pense sont liés à la maladie :
– Je vois des halos lumineux en conduisant la nuit et je suis souvent ébloui par les phares des autres voitures
– Je vois des corps flottants, en particulier sur mon oeil gauche quand je me concentre sur fond blanc.
Ma question est : Est ce qu’il y a des moyens/traitements qui permettent de diminuer, voire de faire disparaître ces phénomènes?
Merci d’avance pour votre réponse.
Bien cordialement.
La corrélation entre l’oeil le plus atteint et la position de sommeil est effectivement frappante, et c’est un argument lourd en faveur de l’origine mécanique du kératocône. Je ne suis pas certain que la pression de l’oeil contre le matelas ou l’oreiller soit la cause directe de la déformation. En revanche, elle favorise l’émergence de nombreux facteurs de risque de frottement : irritation locale, chaleur, contamination par les acariens de literie, germes divers etc. Nous avons étudié la position de sommeil chez les sujets non atteints de kératocône (déclarant ou non se frotter les yeux), et nous en avons plutôt déduit qu’en l’absence de frottements associés, il n’y a pas de kératocône ches les sujets qui dorment « sur l’oeil » mais ne se frottent pas les yeux. Il est toutefois préférable de corriger ce facteur dans votre cas, car il est possible que des frottements réflexes soient effectués pendant le sommeil ou des phases d’éveil rapide. Vous pouvez également porter une coque de protection pendant une nuit ou deux, ce test est assez instructif, car les patients qui se frottent les yeux de manière réflexe en prennent alors conscience (la coque s’interpose entre les paupières et les doigts). Concernant l’évolution de votre kératocône, celle-ci ne doit pas être une simple « impression » mais documentée de manière aussi précise que possible avec des cartes topographiques différentielles. Il existe des fluctuations de mesure entre divers examens, et de fait il est important de ne pas poser le diagnostic de progression par excès. Nous n’avons jamais observé de progression d’une déformation quand les patients cessent réellement de se frotter (je vous invite à consulter le site http://www.defeatkeratoconus.com pour prendre connaissance de ceci si ce n’est déjà fait). Enfin, de mon point de vue, la correction d’une myopie légère par la technique de PKR (laser de surface) est tout à fait possible pour les formes peu évoluées et non évolutives (c’est à dire quand le problème des frottements est définitivement réglé).
Bonjour Docteur,
J’ai lu tout ce que vous avez pu rédiger sur le kératocône depuis déjà un moment. J’ai été diagnostiquée il y a 4 ans, suite à un test pour une chirurgie pour la myopie. Le premier ophtalmo l’ayant détecté voulait bien m’opérer et réaliser un cross-linking en même temps…et proposait de faire cela rapidement. Angoissée par cette nouvelle , j’ai été consulter en clinique universitaire chez une spécialiste où je suis suivie depuis lors. Celle-ci ne préconise pas d’opération de la myopie sur un oeil « malade ». Par contre elle m’a confirmé lors de ma dernière consultation que mon kératocône était toujours légèrement évolutif, alors même que j’ai stoppé les frottements à l’oeil comme elle me l’avait d’ailleurs dit, dès la première consultation, il y a +- 4 ans. J’ai un peu d’astigmatisme à présent en plus de la myopie. Elle m’a dit qu’il faudrait « un jour songer à l’opération du cross-linking » avant que cela ne se dégrade plus. J’avoue être échaudée par tous ces diagnostics et avoir développé la peur qu’on m’opère/touche à mes yeux. Ayant arrêté les grattements, je pense donc que c’est ma position de sommeil qui favorise une compression de l’oeil. J’essaie autant que possible de dormir sur le dos mais je dors régulièrement sur le côté gauche (oeil effectivement le plus atteint) sur un oreiller ferme ergonomique. Si cette pression favorise le développement du kératocône, que puis-je donc faire, quel type d’oreiller choisir? Je précise aussi que je suis sujette aux allergies saisonnières et que j’ai eu une grossesse (influence des hormones?) En vous remerciant,
Bonjour,
J’ai 30 ans et ai un kératocone déjà bien avancé. Est-ce que lorsque j’aurai 90 ans si j’atteins cet age je serais très certainement aveugle à l’oeil le plus détérioré, même si je le stabilise ?
Bonjour Dr,
Je viens de m’equiper de lentilles rigides en piggy-back ( avec lentilles souples ),
Ma question est comment choisir les lentilles souples? de quelle puissance? de quelle type?
Merci
Mon expérience étendue me permet de vous affirmer que l’arrêt des frottements oculaires permet à lui seul de stopper l’évolution de la déformation cornéenne. On vous proposera ici et là des techniques comme le cross linking, mais une étude non biaisée des résultats de la littérature et un esprit un tant soi peu scientifique (et dénué d’arrières pensées commerciales) suffit à reconsidérer cette technique, qui n’a toujours pas bien fait la preuve de son efficacité première, ce pour quoi elle est conçue, c’est à dire rigidifier la cornée. Cela paraît curieux, voire inquiétant, de penser que l’on puisse proposer à des patients une technique si faiblement efficace (et non dénuée de complications), mais c’est comme cela… Encore une fois, et comme vous l’avez constaté, l’arrêt des frottements stabilise le kératocône, à n’importe quel âge. Faites attentions au moments de la journée comme le réveil, ou la douche, pendant lesquels les patients se frottent parfois les yeux à leur insu.
Ce genre de technique, qui permet d’éviter de frotter l’oeil et appuyer sur la cornée, est nettement préférable à celle qui consisterait à « appuyer » et frotter vigoureusement.
En pratique, la gestion éclairée du kératocône permet d’éviter les complications sévères et de devenir aveugle. Le seul traitement pleinement efficace pour stopper l’évolution du kératocône est l’arrêt des frottements oculaires. C’est à la fois simple, et compliqué (il est parfois difficile de résister à la tentation de se frotter le yeux irrités).
Le keratocone peut il rendre aveugle ?
J’ai une autre question docteur, quand mes yeux me grattent ou que j’ai une poussière je ne me frotte pas les yeux mais j’ai une technique qui consiste a » tirer » mes cils ce qui me soulage un peu . Je fais attention a ne pas mettre de forte pression sur la cornée .
Pensez-vous que je devrais arrêter ?
Bonjour Dr,
je voudrais savoir si le fait que je ne porte pas mes lentilles SPOT aggrave mon kératocone ?
Je deteste les lentilles et les supporte mal, néanmoins j’arrive a me débrouiller sans lentilles avec une vie a peu près normale ( même si c’est compliqué parfois ) , je m’y suis habitué .
Je pense que mon keratocone s’est relativement stabilisé depuis que j’ai arrêté de me frotter les yeux .
J’ai une autre question : est ce vrai que le kératocone arrète d’évoluer après 30 ans ?
Merci pour votre réponse .
Cordialement .
Bonjour,
Je souhaitais savoir pourquoi le kératocone est rare chez les personnes hypermétropes ? Le kératocone est il aussi évolutif que pour ceux atteints de myopie ? Merci par avance. Cordialement. Jessie.
Non, le kératocône n’est pas une maladie infectieuse ni lié à la méningite. C’est une maladie plurifactorielle, principalement liée à la réalisation de frottements oculaires répétés et vigoureux (donc plus fréquente chez les patients allergiques, ou sujets à la fatigue chronique, au travail sur écran prolongé, etc.).
Cette maladie est est-elle due à une sur méningite, avec élévation de la température?
Tout d’abord bravo pour l’arrêt des frottements qui expliquent la survenue de la déformation cornéenne. Ne plus frotter permettra à votre cornée d’être stable. Concernant les halos, ceux-ci devraient en principe être réduits avec les lentilles (si celles-ci sont rigides), en particulier les déformations lumineuses asymétriques (traînées lumineuses, spicules, rayons en étoiles partant vers le bas, etc.). Cependant, la disparition totale des halos est difficile pour plusieurs raisons; citons le fait que certaines aberrations ne sont pas complètement réduites par les lentilles (notamment l’aberration sphérique qui est parfois même augmentée de manière paradoxale, en raison d’une asphéricité imparfaite de la lentille). Par ailleurs, la déformation conjointe de la face postérieure de la lentille induit des aberrations (qui sont orientées « à l’envers des aberrations de la face avant de la cornée et tendent à réduire un peu le taux global des aberrations optiques d’origine cornéenne). Quand vous portez les lentilles, la face avant est « corrigée », mais ceci démasque la déformation de la face arrière de la cornée. Si vous observez que la direction dans laquelle la lumière « bave » sans lentille (généralement plutôt vers le bas) est inversée avec la lentille (léger décalage vers le haut), alors cette dernière hypothèse pourrait être accréditée.
Bonjour Docteur,
Je me permets de vous contacter car diagnostiqué avec un kératocône je vois des halos autour des sources lumineuses rendant la conduite difficile surtout de nuit, on m’a donné des lentilles de contact spéciales qui rendent ma vue très bonne cependant les halos ne sont que légèrement modifiés, que dois je faire pour améliorer ce problème ?
J’ai arrêté les frottements qui pourraient être la cause du kératocône. (prurit le matin dans l’oeil)
Merci par avance.
Répétons que le kératocône étant selon moi une déformation secondaire à des frottements excessifs (dont l’énergie finit par vaincre la résistance ou limite d’élasticité de la cornée), seuls les frottements sont à même de faire évoluer cette déformation, et donc ce que l’on appelle « kératocône ». L’air sec est une source d’irritation oculaire, et en ce sens peut conduire à avoir envie de se frotter les yeux. Il faut absolument cesser cela et simplement instiller des collyres mouillants régulièrement.
Merci beaucoups Dr,
Cette question est importante pour moi : Etant un ingenieur informatique (developpeur de logiciels) travaillant en Arabie Saoudite a Riyadh ou le climat est tres sec, est ce que cela peut agraver la maladie?
Merci
Il n’est pas possible de définir un stade de kératocône à partir de ces informations. La notion de stade est toutefois arbitraire. Il est plus intéressant de classer le kératocône en fonction de la gêne fonctionnelle engendrée. Si vous êtes adaptable en lentilles rigides, c’est une donnée essentielle car elle vous permet en principe de vivre relativement « normalement ». Les anneaux cornéens permettent, quand l’amélioration est effective, de réduire l’astigmatisme cornéen, mais ils ne peuvent solutionner tous les problèmes optiques posés par la déformation de la cornée. Ils peuvent effectivement occasionner des symptômes visuels indésirables quand la pupille se dilate, c’est à dire dans les situations de faible luminosité (pénombre, conduite de nuit, etc.). Au risque de me répéter, le plus important dans un premier temps est de ne plus vous frotter les yeux, et d’essayer de vous faire adapter en lentilles de contact rigides. En ce qui concerne l’évolution potentielle du kératocône, il serait intéressant de réaliser des cartes différentielles entre les examens réalisés à ces différentes dates.
Bonjour Dr,
Merci pour cet article tres interessant.
En effet je suis atteind par une keratocones un peut evoluee, et j’ai quelques questions :
1-Etant un ingenieur informatique (developpeur de logiciels) travaillant en Arabie Saoudite a Riyadh ou le climat est tres sec, est ce que cela peut agraver la maladie?
2 – j’ai fait deux topographies corneennes ( difference 6 mois ) :
– la premiere a 29/06/2016 : OD Simk -6.4 D max 47.6 D thinnest 421 um / OS SimK -7.4 D max 52.4 D thinnest 383 um.
– la deuxieme 05/02/2017 : OD Simk max 52.1 D thinnest 431 um / OS SimK max 53.9 D thinnest 423 um.
Puis-je savoir a quelle stade je suis?
Est ce que les anneaux seront une bonne solution dans mon cas?
J’ai entendu parler que les anneaux sont tres genants la nuit surtout avec les lumieres de voitures, est ce que c’est vrai?
Merci beaucoups
Les risques d’abcès sont faibles avec les lentilles hybrides si vous respectez les règles d’entretien et de port. Le confort des lentilles hybrides est supérieur à celui procuré par les lentilles rigides a priori.
Bonjour docteur, déjà merci pour cet article concernant le keratocone et également pour le temps que vous consacrez a répondre a nos questions.je suis actuellement atteins d’un keratocone bilatérale, et aux stades 3 (og/od),et on m’a prescrit des lentilles hybrides lcs,car je supporte mal les menicon rigides. Pouvez vous m’en dire plus sur les hybrides, surtout les inconvénients, parait il qu’il peut y avoir un abcès de la cornée, a cause du matériau de celle-ci(pas assez oxygéné) ?merci,bonne continuation, dans le domaine médical et même privé.
Les chiffres que vous rapportez sont effectivement très évocateurs de kératocône. Dans cette configuration, il convient de cesser de se frotter les yeux (définitivement) et de tenter une adaptation de lentilles de contact rigides. Consultez ce lien : https://www.gatinel.com/2016/12/faire-devant-decouverte-dun-keratocone/
Bonjour docteur. Je suis tombée sur votre site en recherchant des informations concernant le keratocone. J’ai lu tout votre article et c’est vraiment intéressant. J’ai fait une topographie cornéenne et c’est mentionné « Aspect clinique d’un keratocone ODG avec astigmatisme moyen de 8,89 OD et de -10,11 OG.
OD: Simk à 60,81 astigmatisme 8,89
OG: Simk à 60,48 astigmatisme-10,11 »
Je ne verrai le médecin que la semaine prochaine et j’aimerais connaître le type de keratocone que j’ai (s’il est à un stade grave ou non) et le meilleur traitement à adopter selon vous. A savoir que j’ai une myopie très forte qui ne pouvait pas être corrigée d’après plusieurs ophtalmologistes. Merci d’avance
Le diagnostic du kératocône repose sur la réalisation d’une topographie cornéenne. Cet examen permet d’apprécier la forme de la cornée, son épaisseur, et sa régularité. Le kératocône est caractérisé par une déformation de la cornée, qui peut donner (ou augmenter) la myopie, et l’astigmatisme. Sans topographie, il est difficile d’affirmer qu’il existe un kératocône, même si le contexte clinique peut être évocateur. De mon point de vue, le mécanisme de la déformation de la cornée est directement lié aux frottements oculaires. La première chose à faire est d’arrêter de se frotter les yeux et faire des contrôles à intervalles régulier. Les patients qui ne se frottent plus les yeux ne progressent plus. voir ici : https://www.gatinel.com/2016/12/faire-devant-decouverte-dun-keratocone/
Bonjour
Mon ophtalmologiste m’a parler d’un keratocone. Il n’est pas sur de lui et était en retard dans ces rdv et donc ne pas plus expliqué. Il a fait un courrier pour un specialiste en indiquant qu il n y avait pas d opacités de la cornée et les fonds oeils sont normaux mais un aspect de KC et mon acuité visuelle est corrigée à 6/10 au max pour les deux yeux.
Il m’a quand meme prescrit des lunettes.
OG -3,50 (-4,50 à10°)
OD -4,75(-5,00 à 163°)
C est la premiere fois que je change de lunette en 3 ans.
J’ai 31 ans et j’ai peur au vu des messages et remoignages que j’ai pu lire.
Est ce vraiment un Keratocone?? Peut il evolué rapidemnet à mon age ??
Merci de votre rèponse
Si les anneaux sont mal tolérés localement, il est effectivement indiqué de les retirer. Il est indiqué de réévaluer l’intérêt d’une nouvelle adaptation contactologique, car des progrès ont été accomplis dans le domaine des lentilles destinées à la réhabilitation visuelle des patients atteints de kératocône.
Bonjour et merci pour ce forum
J’ai 42 ans et ai subi une pose d’anneaux sur l’oeil droit en 2001 me permettant de retrouver une vue correcte 7/10ième.
Aujourd’hui mon oeil semble faire un rejet, nécessitant un retrait.
Quelles solutions se proposent à moi pour retrouver une vue correcte. Puis-je envisager de nouvelles lentilles. Les derniers tests en 2000, n’avaient pas été concluant me provoquant de fortes irritations.
Y a t’il eu des évolutions à ce sujet ?
Je vous remercie par avance pour votre réponse
Bonjour Docteur Gatinel , j’ai besoin de vos réponses. Votra assistant Docteur Saad m’a diagnostiqué un début de kératocone il y a deux mois et prescrit une adaptation aux lentilles rigides avec le docteur VAYR. Etant de Rouen , je l’ai faite hier à Rouen. Seulement voila on me dit que mes yeux ne les supportent pas après 3 modèles différents et on me laisse repartir sans rien me dire. Je dois alors laisser ma vue baisser comme ça sans rien pouvoir faire pour me soulager ? J’avais l’impression de les supporter comment peut on voir que mes yeux eux non ? Je pensais qu’il y avait forcément un modèle de lentilles nous correspondant ? Je pensais aller voir le docteur VAYR pour un deuxieme avis mais j’ai peur d’avoir la même réponse. Que dois je faire pour soulager ma vue floue sachant que mes lunettes ne me corrigent presque plus ? Merci d’avance
Cordialement
Jessie 25 ans.
L’arrêt des frottements interrompt le mécanisme à l’origine de la déformation cornéenne, mais malheureusement celle-ci est définitive. Parfois, on observe cependant une petite amélioration quelques semaines après l’arrêt des frottements, probablement grâce à un léger remodelage épithélial.
Est-ce que la cornée qui est un tissus, peut se régénérer si la déformation n’est pas trop importante et que je ne me frotte plus les yeux ?
Je vous remercie de votre question, et de ne pas trouver absurde l’idée que la déformation cornéenne observée au cours du kératocône soit la conséquence directe des frottements oculaires. A dire vrai, il est de mon point de vue absurde de prétendre que la cornée puisse se déformer sans l’action d’une force mécanique externe (les frottements), alors que l’on a jamais mis en évidence de mécanisme biochimique, de mutation responsable d’une anomalie protéique ou autre. Ceci a son importance, car dans votre cas, si l’oeil droit est indemne de kératocône (absence de déformation ou déformation minime), et que vous avez cessé de vous frotter les yeux, alors il n’est pas incongru de mon point de vue de vous proposer une technique de correction de la myopie, plutôt en PKR. Si vous avez frotté les yeux dans le passé, vous avez peut être fragilisé la cornée du côté droit, donc il me parait préférable d’opter pour une technique de laser de surface (PKR), si toutefois celle-ci est possible – et un bilan topographique avec mesure de votre correction à délivrer pourra peut être confirmer ceci.
Bonjour,
Je suis atteint de kératocône sur l’œil gauche depuis plus de 20 ans (j’en ai 34 actuellement), il est vrai que je me suis beaucoup frotté les yeux dans ma vie étant allergique au pollen et aux acariens donc l’hypothèse que vous avancez ne me paraît pas absurde.
Sur l’œil droit je n’ai qu’une myopie (bien que lui aussi ait eu droit à sa dose de frottements) et je pensais à me faire opérer au laser mais je ne suis pas sûr que ça soit une bonne idée, cela ne risquerait-il pas de fragiliser la cornée de mon œil droit ?
Vous remerciant par avance de votre retour.
Cordialement,
Laurent
Le port de lentille sclérale est possible en cas de greffe de cornée, sans réduire la durée de vie des greffons, et l’amélioration attendue pour votre vision est a priori substantielle.
Bonjour,
Je suis greffée de la cornée depuis 16 ans pour l ‘ oeil droit et 15 ans pour l ‘ oeil gauche ,effectivement d ‘ aussi longtemps que je me souvienne je me frottais très souvent les yeux,ma vue a dégringolé en un an et demi et suis passée de 10/10 à 1 et 2/10ème en un an et demi ,j’avais 17 ans,je me renseigne depuis qqs temps sur les lentilles sclérales et il semblerait que les lentilles sur greffons réduisent leur durée de »vie ». (Actuellement je porte des lunettes mais ne suis pas à 10,un essai de lentilles sclérales m ‘ a redonné goût à bien mieux voir ),qu’ en pensez-vous?avez vous déjà réalisé des études sur cette question?
Par ailleurs je suis en contact avec des keratoconiens sur fb,qui ont leur source auprès d’ ophtalmos et pour le CXL (crosslinkin) effectivement l’ efficacité est loin d ‘ être prouvée.
En vous remerciant.
Marion
Il n’y a pas de contre indication pour la musculation, ou toute autre activité sportive tant que celle-ci ne vous conduit pas à vous faire vous frotter les yeux. Gares donc aux poussières, ou à la sueur qui coulerait dans les yeux.
Est ce qu’on peut pratiquer la musculation quand on est au stade 3 du kératocône?
Si vous lisez les pages conacrées au kératocône et au crosslinking de ce site, vous pourrez deviner ma réponse à vos interrogations. Premièrement, le kératocône a été provoqué dans votre cas et dans (à mon avis) tous les autres cas par les frottements oculaires. Son évolution, qui doit être jugée sur la réalisation de topographies espacées dans le temps, et dont les différences doivent être significatives, est également liée à la poursuite de ces frottements.
De cette assertion découle une conclusion limpide: si vous cessez strictement de vous frotter les yeux, votre kératocône n’aura plus de raison d’évoluer. De mon point de vue (nourri par la pratique et l’observation et suivi de dizaines de cas de kératocône), le kératocône n’est pas une dystrophie cornéenne dont l’apparition découle d’un terrain génétique favorable et de certains facteurs environnementaux. Son origine est beaucoup plus simple: il est le fruit d’une fragilisation biomécanique de la cornée acquise et directement provoquée par les frottements oculaires répétés, qui provoquent un étirement progressif et une désorganisation des lamelles collagènes de la cornée.
Il n’y a jamais d’urgence à réaliser un CXL car même si l’on croit à l’efficacité de cette technique (non prouvée par les méta analyses sérieuses), il faut réaliser au moins deux topographies à quelques semaines d’intervalle prouvant une progression de l’affection pour poser l’indication de CXL. Si le KC n’évolue pas, pourquoi réaliser une technique consistant à réaliser un stress oxydatif intense destiné à induire d’hypothétiques liaisons covalentes au sein du tissu cornéen? Les modifications apportées par le CXL sont modestes et liées à la cicatrisation de la surface cornéenne, pas à une réelle solidification de celle-ci.
Bonjour,
J’ai 26 ans et on viens de me diagnostiquer un kératocone DPM évolutif d’après le spécialiste.
Un astigmatisme qui a évolué les derniers mois/années.
Je porte actuellement des lunettes ainsi que des lentilles souples pour le sport 4 fois semaines.
Je me frotte régulièrement les yeux. (Fatigue, lentilles, poussière, réveil )
Le chirurgien me propose une opération très rapide via le crosslinking .. Je suis assez méfiant concernant cette technique et surtout l’aspect urgent de l’opération.
Que me conseillez vous ?
Merci
Le port de lentilles rigides bien adaptée n’est absolument pas un risque concernant l’évolution de votre kératocône. La pression exercée par les paupières et transmise à la cornée par la lentille rigide est de plusieurs ordres de magnitude inférieure à celle des doigts ou phalanges lors des frottements oculaires. L’amélioration significative de votre vision grâce aux lentilles est liée au fait que leur géométrie permet de rendre un galbe plus harmonieux à la surface de l’oeil, ce qui permet de réduire considérablement les aberrations optiques qu’inflige, seul, le kératocône.
Dans un premier temps il convient de confirmer le diagnostic de kératocône. Celui-ci peut parfois être porté par excès, en fonction de la carte topographique réalisée, et des critères utilisés pour le diagnostic. S’il s’agit d’un kératocône, il s’agit de mon point de vue des conséquences d’un traumatisme répété de cos cornées, qui doit être plus fréquent et prononcé du côté le plus atteint; les frottements oculaires répétés sont bien sûr le mécanisme le plus souvent retrouvé. Plus le kératocône apparaît tard au cours de l’existence, et plus son évolution est réputée lente. Il s’agit certainement d’un biais d’appréciation; quand le kératocône apparait tard (ex: après 30 ans), c’est qu’il découle d’un processus lui même d’évolution lente, et qui mène donc plus tardivement à l’éclosion de la maladie. Vous n’avez donc pas forcément à redouter le pire. Ne vous frottez plus les yeux, et faites une autre topographie cornéenne dans quelques mois.
Bonjour Docteur,
Je suis expatrié, ma acuité visuel s’est détérioré en quelques temps. Je suis allé faire des examens, on m’a diagnostiqué un kératocône. Pour le moment seul mon œil droit est atteint, on m’a parlé d’un kératocône frustre à gauche. Je redoute le pire, j’ai toujours une bonne vue, ancien sportif de haut niveau, vie saine. Je ne sais pas trop comment m’y prendre.
Suis-je condamné à moins bien voir ?
bonjour je suis atteint de keratocone depuis 6 ans. On m’a proposé un crosslinking mais depuis que j’ai lu votre site très bien fait je ne me frotte plus les yeux ce que je faisais depuis l’enfance (J’ai 29 ans). Mon keratocone n’évolue plus d’après un autre Opthalmo qui a donné des lentilles rigides. Je vois mieux qu’en lunettes mais est ce que le port des lentilles dures est mauvais en cas de keratocone pour la cornée? Merci
Il est très important que votre fils ne se frotte plus les yeux, sous peine d’induire une récidive du kératocône. Si les frottements sont liés à une allergie, il faut tenter une désensibilisation et traiter les symptômes de l’allergie par des collyres (anti histaminiques) ou des traitements per os. Plutôt que de frotter quand les yeux sont irrités, il est préférable de bien les rincer avec du sérum physiologique. La pratique de la musculation est possible. Concernant la transmission du kératocône, il est classique de considérer cette maladie comme génétique, car on observe parfois la présence d’un kératocône chez plusieurs membres d’une fratrie, chez l’un des parents biologique, etc. Toutefois, le mode de transmission n’est pas clair et il n’y a pas de gène spécifiquement identifié pour le kératocône. Il est en revanche probable que certains traits génétiques prédisposent à avoir un terrain atopique, des cornées plus ou moins épaisses et résistantes… et que la pratique de frottements oculaires induise plus vite un kératocône chez certains sujets que chez d’autres. De mon point de vue, l’absence de frottements oculaires (ou de l’application répétée de contraintes mécaniques sur la cornée) devrait à elle seule suffire à éradiquer le kératocône. Même si l’on est en droit de douter de cette assertion tant les traités définissent classiquement le kératocône comme une dystrophie cornéenne dont l’origine est inconnue, il est admis que les frottements oculaires répétés accentuent la déformation cornéenne et accélèrent l’évolution de la maladie (de mon point de vue, les frottenents sont LA cause de ce qu’on appelle le kératocône et leur intensité et fréquence en conditionnent l’évolution)
Bonjour
Mon fils a la maladie « kératocône », il a eu une greffe les deux yeux depuis 7 ans. Il a de déficit visuelle. Il ne supporte pas de lentilles, puisque à chaque fois qu’il met de lentilles, ça lui gratte beaucoup les yeux, ils sont rouges. C’est la raison qu’il ne met rarement de lentilles.
Depuis quelques temps, il ne voit de moins en moins bien et gratte beaucoup les yeux.
J’aimerais savoir quels sont les gestes à éviter pour minimiser les risques de déficit visuelle de plus en plus grave ?
S’il existe de médicament ou traitement pour nettoyer ses yeux ou éviter de les gratter?
Qu’est ce qu’il faut faire et ce qu’il faut pas faire ou il n’y a pas de solutions vu la gravité de ses yeux. (j’incite qu’on voit très biens les traits blanc sur ses yeux après opérations les deux yeux)
Est ce que cette maladie est transmissible à ses enfants ?
Est ce qu’il doit éviter ou pas forcer sur la musculation car il en fait beaucoup
Je vous remercie pour votre réponse
La pratique de la boxe et des sports de combats est possible en cas de kératocône; il convient comme toujours de protéger les yeux contre les coups portés en direct.
Dans un premier je tenais à vous remercié pour toutes les informations que vous donnez sur le Kératocône, cela m’a permis de rassurer certaine craintes.
J’aurais aimez savoir si les sports de combat type boxe peuvent être pratiqués lorsque nous somme atteints du Kératocône ?
Cordialement,
Je préconiserais le port de lentilles ou de lunettes effectivement. Le kératocône est à un stade avéré mais a priori un équipement en lentilles rigides devrait permettre de remonter l’acuité visuelle corrigée à un niveau satisfaisant.
Il est bien entendu crucial de cesser tout frottement oculaire. Si cette préconisation est respectée, le kératocône ne devrait plus évoluer. Une greffe ne me parait pas devoir être envisagée dans le futur.
Avec l’accord de ma fille, je me permets de vous contacter à son sujet. Agée de 31 ans, elle a consulté récemment un ophtalmologue suite à un ressenti de fatigue oculaire. Le diagnostic préalable a été « astigmatie sévère » puis a été remplacé brutalement par « maladie des yeux : kératocône ». Devant l’inquiétude de ma fille sur la perte de la vue, le médecin a adouci le trait en disant qu’il n’y avait rien de grave : au mieux elle aurait des lunettes, au pire une chirurgie. La spécialiste rencontrée lui propose un cross linking, sans expliquer la maladie et son évolution et sans expliquer pourquoi une solution alternative telle que lunettes ou lentilles ne peut être envisagée. Ma fille refuse cette méthode.
Elle est consciente que sa vue puisse diminuer et est parfois gênée par la lumière trop vive mais elle reste surprise d’entendre que des lunettes ne serviraient à rien alors qu’à ce jour, elle lit de très petits caractères. Elle admet avoir besoin et est prête à porter des lunettes ou lentilles bien qu’elle pense ne pas avoir assez de larmes pour supporter ces dernières.
Pour information, ma fille avait consulté un ophtalmogue à 18 ans pour des raisons de migraines ophtalmiques ; celui-ci n’avait rien diagnostiqué de tel et avait juste préconisé des sessions d’orthoptie. Une fois les séances faites, ma fille n’a plus ressenti de fatigue oculaire jusqu’à récemment.
La lecture de vos articles concernant le cross linking et le kératocône apporte des réponses et confirme l’inquiétude sur cette technique trop souvent proposée dès la première consultation.
Je découvre que le kératocône est souvent provoqué par les frottements oculaires et répétés des yeux, pratique exercée depuis de nombreuses années par ma fille. Elle manque également de larmes (sécheresse oculaire) qu’elle compense par des gouttes. Suite à cette annonce, elle ne se frotte plus les yeux car souhaite stopper l’évolution du kératocône.