Ectasie Cornéenne
Ectasie cornéenne : introduction
L’ectasie cornéenne induite (ou kératocône iatrogène) est une complication rare du LASIK qui met en jeu la fonction visuelle. Son début parfois insidieux et retardé dans le temps, son caractère non réversible et son pronostic péjoratif (elle peut motiver l’indication d’une greffe de cornée) sont autant de caractéristiques qui en font une complication redoutée, et lui confèrent une dimension adverse voire pernicieuse.
Le facteur de risque principal de l’ectasie est la présence d’une forme non dépistée de kératocône infra clinique débutant au niveau de la cornée opérée. Comme pour le kératocône, la notion de frottements oculaires répétés est aussi un facteur de risque, ces frottements ayant mené à la réduction de la résistance cornéenne avant l’intervention, et au décours de celle-ci si les frottements ont été poursuivis.
La topographie cornéenne est un examen indispensable pour éliminer la présence de ce que l’on désigne comme une forme très débutante de kératocône infra clinique, dont le diagnostic repose notamment sur l’identification de variations asymétriques de la courbure cornéenne, et l’utilisation d’indices de dépistage automatisés pour le kératocône.
Selon l’auteur de ce site, la notion de « kératocône fruste » recoupe celle d’un tableau topographique dominé par la présence d’irrégularités cornéennes induites par le stress mécanique répété que constituent les frottements oculaires. En effet, le relief cornéen dépend de ses propriétés structurelles et des forces qui y sont appliquées. Les patients qui frottent régulièrement leurs yeux (allergie, fatigue et sécheresse oculaire) induisent au fil du temps une réduction de la rigidité cornéenne; le traumatisme infligé est source d’un amincissement central ou paracentral et de l’apparition d’une courbure plus irrégulière, ainsi que d’un astigmatisme. L’importance de ces signes est fonction de l’intensité, de la durée et du type de frottement, et des caractéristiques natives des cornées.
Ce tableau représente ainsi une contre indication à la réalisation du LASIK et également à celle des procédures de type SMILE. En effet, ces anomalies topographiques traduisent la réduction de la résistance biomécanique de la cornée.
Dans ce contexte, et pour des myopies faibles et moyennes, les techniques de surface (PKR) peuvent en revanche être réalisées dans certains cas.
Cette page concerne les principales caractéristiques cliniques et topographiques de cette complication : une attention particulière sera donnée à l’étude des facteurs qui en favorisent la prévention.
Diagnostic de l’ectasie cornéenne
Définition de l’ectasie cornéenne
L’ectasie cornéenne induite peut être définie comme l’apparition dans un délai variable après réalisation d’une procédure de LASIK ou de SMILE d’un tableau clinique et topographique de kératocône évolutif. La cornée présente une déformation progressive avec cambrure centrale et irrégularité accentuée.
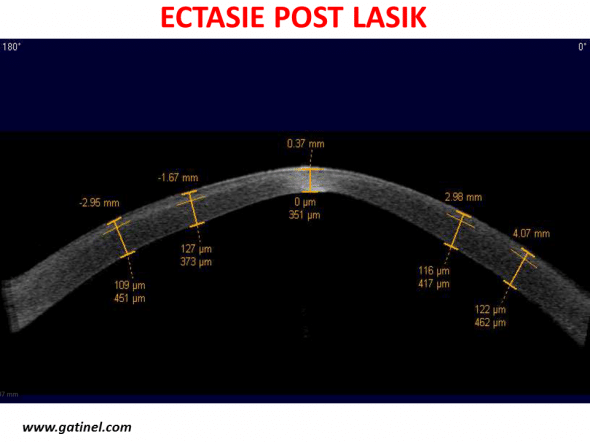
OCT en coupe sagittale d’une cornée présentant une ectasie post LASIK. Noter la déformation centrale avec cambrure accentuée irrégulière. L’épaisseur du capot est estimée à 120 microns en moyenne. Au centre, l’épaisseur du capot semble réduite, et l’épaisseur totale de la cornée est estimée proche de 350 microns.
– Les signes cliniques de cette complication associent une dégradation progressive de la fonction visuelle avec ré-apparition d’une myopie et/ou d’un astigmatisme (astigmatisme de direction souvent oblique), baisse de l’acuité visuelle non corrigée, puis perte de lignes de meilleure acuité visuelle corrigée (MAVC): même avec une correction lunettes, l’acuité visuelle demeure inférieure à 10/10. La survenue d’une ectasie peut intervenir quelque semaines après LASIK, parfois quelques années.
– La topographie cornéenne spéculaire (courbure) révèle l’apparition d’une zone de cambrure élevée généralement localisée dans la moitié inférieure de la surface cornéenne antérieure. L’apparition d’une courbure irrégulière après chirurgie réfractive cornéenne doit toujours faire penser à la possibilité d’une ectasie. L’ectasie est souvent confondue avec un décentrement supérieur.
– La topographie d’élévation souligne une distribution asymétrique de l’élévation de la face antérieure de la cornée et permet de localiser le sommet de l’ectasie qui se situe le plus souvent dans la région centrale ou paracentrale inférieure. L’élévation de la face postérieure vis à vis de sa sphère de référence calculée est souvent très accentuée en regard de la zone de pachymétrie minimale.
– La pachymétrie optique permet le repérage des coordonnées et la valeur du point d’épaisseur minimale du mur cornéen résiduel. Celui-ci est généralement faible, et sa localisation dépend de la position initiale du point le plus fin et du centrage du profil d’ablation. Il est possible que de mécanismes inflammatoires induisent une diminution du nombre de fibres collagènes lors de la survenue d’une ectasie iatrogène de la cornée, et accentuent l’amincissement de la cornée.
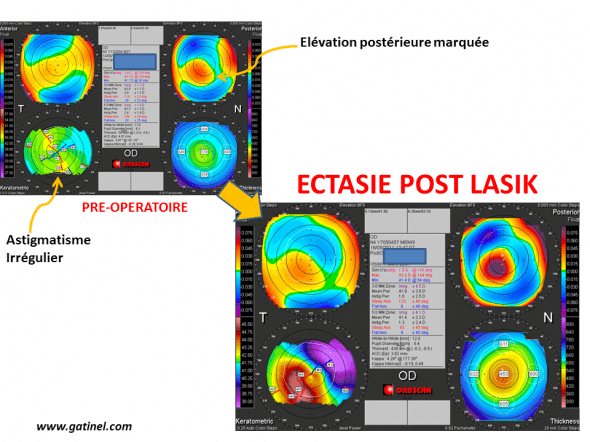
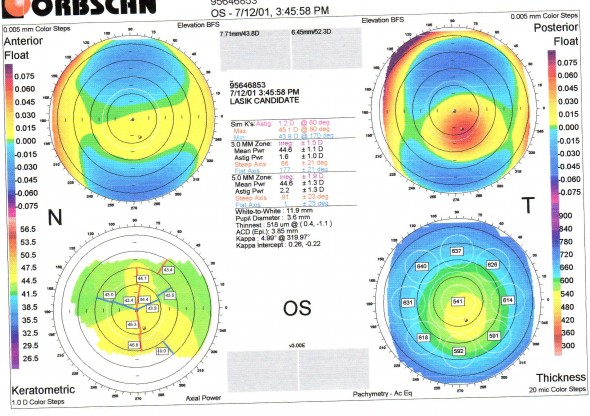
Ectasie apparue deux ans après la réalisation d’un LASIK chez une patiente de 36 ans, pour une myopie d’environ 6 D. En préopératoire, on note un astigmatisme irrégulier de l’œil droit, avec élévation marquée de la face postérieure. Il existait un terrain atopique avec notion de frottements oculaires digitaux répétés. La carte post opératoire révèle un aspect d’amincissement central marqué, avec déformation asymétrique de la face antérieure, et élévation postérieure accentuée
– L’examen aberrométrique souligne l’élévation du taux des aberrations optiques de haut degré. La déformation cornéenne asymétrique provoque une augmentation des aberrations optiques impaires (coma, trefoil). Le taux de ces aberrations s’accroît de façon exponentielle avec le diamètre pupillaire et celles-ci peuvent être responsables d’une diminution de la sensibilité aux contrastes, puis d’une réduction de la MAVC. De même, la sensation d’une « vision dédoublée » au niveau de l’oeil atteint est fréquente.
Il est à noter qu’aucun de ces signes n’est spécifique de l’ectasie cornéenne induite (voir diagnostic différentiel). Leur conjonction et leur aggravation/accentuation avec le temps au décours d’un LASIK est toutefois très évocatrice, et permet d’éliminer la présence d’un décentrement.
Causes et facteurs de risque de l’ectasie cornéenne
Une revue de la littérature concernant l’ectasie cornéenne post-LASIK a été publiée récemment (1). Quatre vingt cinq cas d’ectasie post LASIK ont été analysés. Au terme de cette analyse, la présence d’un kératocône fruste ou avéré était avérée dans environ 28 cas, non documentée dans 18 cas, et considérée comme absente dans les 39 cas restants.
En dehors de l’existence possible de facteur(s) de risque(s) actuellement non identifiés, deux étiologies principales sont classiquement invoquées pour expliquer la survenue d’une ectasie secondaire chez les patients opérés en LASIK : l’amincissement excessif du mur postérieur cornéen chez des sujets normaux, ou la présence d’un kératocône infra-clinique non identifié parmi les cas considérés comme normaux (2). Dans ces deux situations, l’ectasie surviendrait par affaiblissement excessif de la paroi cornéenne avec décompensation biomécanique et /ou au terme de l’évolution d’un processus pathologique progressif accéléré par le LASIK (3).
En effet, l’étude des caractéristiques préopératoires des patients ayant présenté une ectasie après LASIK révèle la présence d’une myopie et d’un astigmatisme plus prononcés que chez les sujets indemnes, ainsi que le calcul d’une épaisseur plus fine du mur résiduel postérieur.
Mécanisme de l’ectasie cornéenne
S’il est logique de postuler que le comportement biomécanique d’une cornée découpée en surface puis amincie chirurgicalement puisse différer de celui d’une cornée saine et vierge sur le plan chirurgical, les éléments impliqués dans le contrôle de la biomécanique cornéenne et le processus conduisant à l’apparition de l’ectasie ne sont certainement pas tous identifiés.
L’étude du mécanisme physio-pathologique de l’ectasie cornéenne fait paradoxalement l’objet de peu d’études expérimentales, qui seraient pourtant nécessaires afin de préciser l’influence de paramètres pré opératoires tels que la kératométrie moyenne, le module d’élasticité de la cornée (module de Young), ou la pression oculaire. Une étude en histologie sur un bouton cornéen trépané avant kératoplastie transfixiante a mis en évidence la présence de macro-stries au niveau du stroma postérieur (4).
La cornée est une coque qui est soumise à une force exercée sur toute sa surface postérieure par la pression qui règne à l’intérieur oculaire, et ses propriétés biomécaniques lui permettent de conserver un galbe harmonieux dans des conditions physiologiques. Il est recommandé, sur la base de données empiriques, de ne pas amincir la cornée de manière excessive en LASIK et de préserver un mur résiduel postérieur stromal d’au moins 250 microns, ou encore de ne pas induire un mur résiduel postérieur inférieur à la moitié de l’épaisseur cornéenne initiale, pour éviter une décompensation biomécanique et l’ectasie.
La technique de SMILE, initialement positionnée comme moins susceptible de provoquer une ectasie, semble à proscrire en cas de doute. Des cas d’ectasie post SMILE ont été rapportés, survenant pour des cornées présentant des atypies topgoraphiques en préopératoire. La communication délivrée autour du SMILE insiste sur l’absence de découpe de capot mais occulte souvent le nécessaire retrait d’un lenticule en profondeur , profondeur d’ailleurs souvent plus importante qu’en LASIK où il est possible de réaliser des capots fins.
Diagnostic différentiel de l’ectasie cornéenne
Le piège diagnostic principal est le décentrement de la photoablation, dont les signes topographiques peuvent être voisins, mais dont les modalités de prise en charge sont évidemment différentes de celle de l’ectasie induite (où toute photoablation complémentaire après re-soulèvement du capot est évidemment proscrite) (Figures 1-3).
Fréquemment, l’ectasie est observée après « retouche » pour une sous correction, ou ce qui était diagnostiqué comme un décentrement.
Tout décentrement et/ou sous correction- régression rapide de l’effet de la correction après LASIK doit être considéré comme une ectasie jusqu’à preuve du contraire.
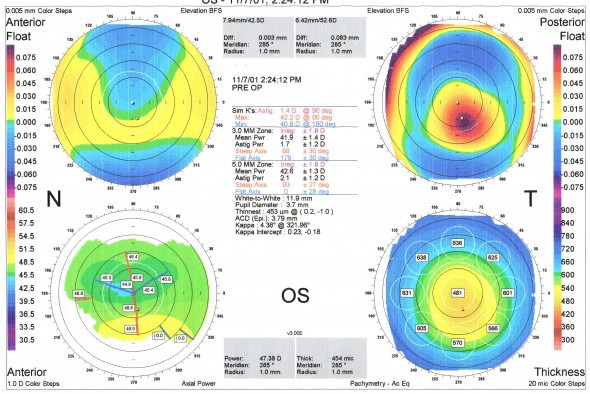
Figure 2 : carte Orbscan postopératoire, sept jours après LASIK ( Hansatome anneau 9.5/ tête 180, photoablation : -5,75 D sur zone optique de 5.5 mm / profondeur d’ablation maximale : 84 microns, Laser Technolas 217)
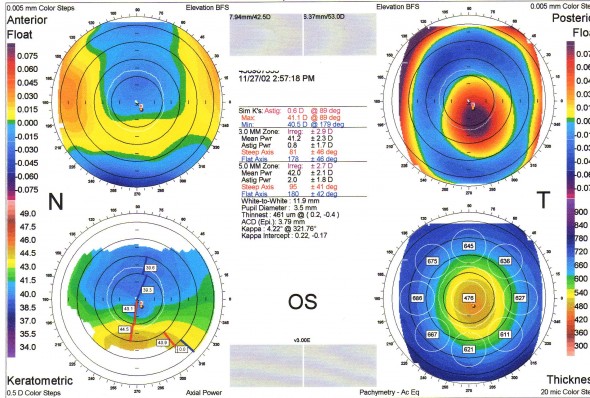
Figure 3 : carte Orbscan effectuée après reprise chirugicale pour décentrement supposé : resoulèvement et délivrance d’une photoablation complémentaire. Noter l’accentuation de l’asymétrie cornéenne et l’accentuation de l’ectasie.
Commentaires :
Ce cas d’ectasie induite survenu chez un patient de 42 ans opéré en LASIK pour une myopie moyenne est particulièrement illustratif. Il présentait avant l’intervention un aspect de kératocône infraclinique non diagnostiqué. L’accentuation de l’asymétrie initiale (qui traduisait la « faiblesse biomécanique » préopératoire liée au kératocône débutant) après la chirurgie a été considérée de manière erronée comme un décentrement supérieur de la photoablation. Il est probable qu’un mur postérieur d’au moins 250 microns ait été respecté dans ce cas, l’ectasie étant la conséquence de la fragilisation excessive du mur cornéen. Dans notre expérience, l’ectasie consécutive à la découpe de cornées « fragiles » survient rapidement après le LASIK, alors que l’amincissement excessif d’une cornée initialement normale survient plus tardivement.
Sur la carte topographique préopératoire (Figure 1) , on note l’asymétrie présente au niveau de la face antérieure, qui est responsable d’un astigmatisme asymétrique en carte spéculaire axiale, et d’une distribution asymétrique de l’élévation. L’échelle utilisée sur la carte spéculaire est toutefois trop large et « écrase » les variations de courbures de la face antérieure de la cornée, ce qui estompe l’aspect asymétrique du sablier vertical.
L’aspect de la carte d’élévation postérieure est particulièrement suspect (élévation accrue et décalée vers le bas vis à vis de la sphère de référence calculée). Enfin, si la pachymétrie moyenne centrale possède une valeur normale (541 microns), il existe un point d’épaisseur minimale (thinnest point) mesuré à 518 microns et dont la localisation est décalée en inférieur. L’ensemble de ces signes évoque rétrospectivement la présence d’un kératocône infra clinique (kératocône fruste voir kératocône suspect). Le patient a été cependant jugé apte à une correction réfractive en LASIK par son chirurgien.
Il est important de considérer que toute irrégularité topographique observée après LASIK effectué sans problème doit faire éliminer la présence d’une ectasie cornéenne débutante.
En cas de doute diagnostique, l’évolution spontanée permet de trancher. En cas d’ectasie débutante, elle se fait toujours vers l’aggravation progressive, alors que le remodelage cornéen cicatriciel permet souvent de réduire les symptômes cliniques et topographiques du décentrement. Les éléments fournis par les examens topographiques et aberrométrique s’avèrent particulièrement utiles dans ce contexte car ils permettent le suivi et la comparaison d’éléments quantitatifs objectifs.
Il est crucial de garder en mémoire que toute régression de l’effet réfractif après correction en LASIK doit faire éliminer le diagnostic d’ectasie induite. J’ai observé de nombreux cas où un début d’ectasie, considéré à tort comme une sous correction ou un décentrement, a fait poser l’indication d’une retouche qui a malheureusement accéléré l’ectasie. L’apparition d’un astigmatisme myopique de direction oblique est particulièrement évocatrice d’ectasie, surtout quand il tend à s’accentuer. L’examen aberrométrique révèle une élévation progressive des taux de coma et trefoil. La réalisation de contrôle répétés dans le temps avec étude de cartes différentielles permet de confirmer ou d’infirmer le diagnostic.
Traitement de l’ectasie
La prise en charge thérapeutique d’une ectasie dépend de sa sévérité et de son retentissement sur la fonction visuelle.
L’arrêt de tout frottement oculaire est crucial.
La correction optique causée par la déformation cornéenne asymétrique est au mieux effectuée par l’adaptation d’une lentille de contact rigide quand cela est possible (5,6). La pose de segments d’anneaux intra-stromaux, initialement proposée pour le traitement du kératocône (7), représente également une alternative intéressante à la greffe de cornée en cas d’ectasie induite (8). La pose de sutures entre le capot, le stroma postérieur et l’anneau limitant pourrait permettre dans certains cas de limiter l’évolution de l’ectasie (9).
La réalisation de techniques de cross linking (polymérisation du stroma cornéen par application de riboflavine A et l’exposition aux UVA) est une technique dont les effets bénéfiques restent à démontrer, en particulier dans le cas de l’ectasie après LASIK. La stabilisation revendiquée est difficile à caractériser, dans un contexte ou la réalisation du CXL modifie la topographie de la cornée (repousse épithéliale), et que l’arrêt des frottements oculaires est en soi un moyen efficace de ne pas accentuer la déformation de la cornée.
L’insertion de segments intra cornéen (anneaux) permet une certaine réhabilitation visuelle pour certains patients. L’échec des méthodes précédemment citées conduit à envisager la réalisation d’une kératoplastie transfixiante, ou lamellaire profonde, dont les modalités et le pronostic sont similaires à celui du kératocône primitif.
Prévention de l’ectasie cornéenne induite par le LASIK
Les possibilités thérapeutiques étant actuellement limitées en matière d’ectasie induite, la prévention de cette complication possède une importance capitale. Elle repose sur deux piliers : le respect d’un mur postérieur résiduel d’épaisseur résiduelle suffisante, et SURTOUT l’exclusion des cornées « à risque ». Par ailleurs, il est important d’expliquer au patient qu’il ne faut se frotter vigoureusement les yeux sous aucun prétexte après chirurgie réfractive cornéenne; les frottements oculaires répétés favorisent le déclenchement et l’évolution du kératocône et de l’ectasie cornéenne.
Voir : Détection des formes précoces de kératocône (kératocône frustres)
Limiter l’amincissement du mur postérieur en LASIK :
La détermination de la valeur minimale de l’épaisseur du mur résiduel stromal à préserver n’est pas déterminée avec certitude. Différentes valeurs ont été proposées, comprises entre 200 et 300 microns ou égales à la moitié de la pachymétrie centrale initiale. Un consensus autour d’une valeur de 250 microns semble se dégager pour l’épaisseur stromale postérieure à préserver (1). En fait, cette valeur dépend de multiples facteurs et demeure certainement spécifique pour chaque patient (10).
Le calcul du mur postérieur résiduel et le choix d’une limite à ne pas franchir concernent uniquement les sujets exempts de fragilité biomécanique cornéenne préexistante.
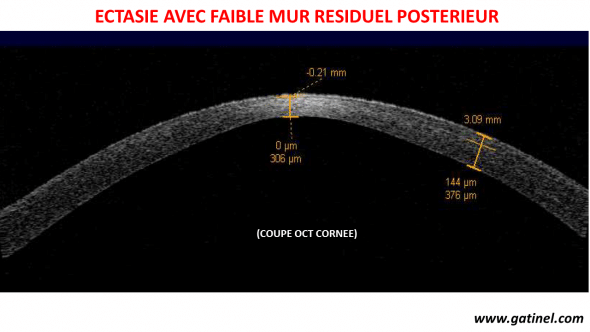
Image en coupe OCT du mur cornéen d’un oeil atteint d’ectasie après LASIK. En périphérie, l’épaisseur du capot est mesurée à 144 microns, alors que l’épaisseur de la cornée au centre est de 306 microns. Le mur résiduel postérieur est estimé à environ 150 microns, ce qui est insuffisant pour maintenir l’équilibre biomécanique du dôme cornéen.
L’existence d’un kératocône fruste traduisant une fragilité structurelle de la paroi cornéenne, la réalisation d’un volet même fin est à proscrire car susceptible d’entraîner, avec la délivrance de la photoablation, une décompensation biomécanique.
Le calcul théorique de l’épaisseur dur mur résiduel postérieur dépend de la pachymétrie initiale, de l’épaisseur prédite du capot et de la profondeur maximale annoncée de photoablation. Il existe toutefois une importante dispersion autour de la valeur prédite moyenne de l’épaisseur des capots obtenus avec la plupart des microkératomes mécaniques de première génération (Automated Corneal Shaper * – Bausch and Lomb, One*, Cariazo Barraquer* manuel et électrique- Moria). L’épaisseur du volet cornéen retenue pour le calcul du mur postérieur peut s’éloigner significativement de l’épaisseur réellement obtenue après découpe mécanique, comme l’ont démontré plusieurs études utilisant une mesure pachymétrique peropératoire (11,12) Par exemple, des volets d’une épaisseur égale à 220 microns ont pu être obtenus …pour une épaisseur escomptée de 160 microns. Un cas d’ectasie immédiate après découpe d’un volet excessivement épais sans photoablation au décours d’une procédure de LASIK avortée (erreur de montage du microkératome) a même été rapporté ! (13)
Calculée à partir de l’épaisseur théorique prédite du capot, l’épaisseur du mur postérieur résiduel aurait ainsi pu être surestimée dans certains cas d’ectasie cornéenne sans violation « apparente » de la règle des 250 microns. Cependant, plusieurs cas de LASIK avec mesure réelle de l’épaisseur du volet permettant le calcul avec d’un mur résiduel postérieur inférieure à 250 microns ont été suivis pendant plusieurs années sans qu’une ectasie ne se développe (14).
La réduction de la dispersion autour de la valeur prédite d’épaisseur et une régularité accrue de découpe font partie des bénéfices escomptés de l’utilisation du laser femtoseconde en LASIK. En effet, la précision de l’épaisseur du capot découpé par le laser femtoseconde est meilleure que celle des microkératomes.
En pratique, la réalisation d’une mesure pachymétrique peropératoire est recommandée quand le calcul théorique du mur postérieur fournit une valeur proche de la limite imposée. Elle consiste à pratiquer une mesure de l’épaisseur cornéenne centrale avant puis après découpe et soulèvement du volet, l’épaisseur de celui-ci étant calculée comme la différence entre les deux mesures précédentes. Le laser EX500 est muni d’un système de mesure de l’épaisseur de la cornée en temps réel (OCT online).
Si la découpe obtenue s’avère plus épaisse que prévue, la réduction de la zone optique programmée pour la correction excimer peut permettre l’obtention d’un mur résiduel suffisant par le biais d’une réduction de la profondeur maximale de photablation (une réduction d’environ 30% est par exemple obtenue en réduisant le diamètre de zone optique de 6 à 5 mm pour une même magnitude de traitement).
En cas de reprise pour sous-correction, une sécurité accrue pourrait être obtenue grâce à l’utilisation de techniques d’imagerie permettant la visualisation fine et la mesure des épaisseurs respectives des différentes tuniques de la paroi cornéenne. L échographie ultrasonique à haute fréquence, ou l’étude en « Optical Coherence Tomography » (OCT3) du segment antérieur permettent l’estimation directe de l’épaisseur du volet et du mur postérieur résiduel obtenu après le LASIK initial. Celle-ci permet alors d’établir la valeur maximale de profondeur d’ablation additionnelle autorisée pour une valeur limite d’épaisseur du mur postérieur résiduel données.
La détection des formes frustes de kératocône et des cornées « à risque biomécanique pour le LASIK »
La détection du kératocône infra-clinique débutant doit être une préoccupation quotidienne en chirurgie réfractive. La fréquence du kératocône infra clinique débutant est plus élevée dans la population de myopes candidats à une chirurgie réfractive (2 à 5%) que dans la population générale (0,05%), en raison d’un biais de sélection lié à l’intolérance fréquente aux lentilles de contact et à la mauvaise qualité de vision obtenue par correction additive chez ce type de patient.
Le diagnostic des formes avérées et évoluées de kératocône ne pose pas de problèmes en vidéokératoscopie spéculaire.
En revanche, il est plus difficile d’éliminer la présence d’une forme débutante de kératocône, dont le diagnostic doit faire récuser le LASIK (10,15). En effet, le kératocône infraclinique (kératocône dont seul la topographie cornéenne trahit l’existence) correspond à une cornée « fragile » sur le plan biomécanique et comme déjà souligné, le passage d’une forme fruste vers une forme avérée (ectasie) peut être accéléré par la simple réalisation d’une découpe cornéenne de capot sans photoablation laser.
A ce jour, la limite précise entre cornée « normale » et « présentant un stade précoce de kératocône » demeure floue. Étiqueter « kératocône fruste » toute cornée présentant des caractéristiques topographiques comme une asymétrie modérée ou une épaisseur inférieure à la moyenne constitue certainement un « abus sémantique ». L’association entre frottements oculaires, ou compression prolongée de la ou les cornées lors du sommeil (patients dormants sur le ventre ou le côté, la tête dans l’oreiller), et les formes « suspectes » de kératocône est troublante.
Nous consacrons une part importante de notre travail de recherche pour prévenir l’ectasie post LASIK, et ces efforts ont été récemment récompensés par des prix internationaux et incarnés dans un logiciel d’aide à la décision clinique, utilisant les données de la topographie cornéenne Orbscan IIz pour un meilleur dépistage des formes infracliniques débutantes (SCORE Analyzer). L’exemple suivant de carte « score » correspond à la cornée ayant présenté une ectasie présentée plus haut. Le calcul du score a bien entendu été effectué de matière rétrospective (le score n’existait pas au moment ou cet oeil a été opéré).
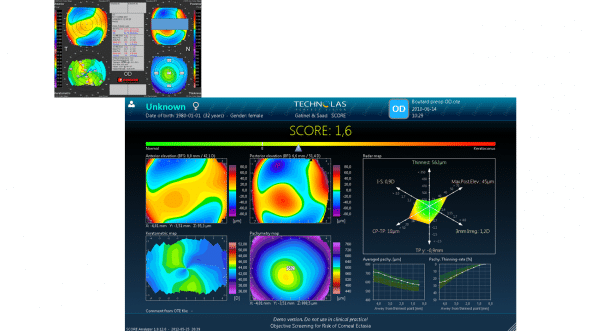
Carte « Score analyzer », obtenue de manière rétrospective pour une cornée ayant présenté une ectasie post LASIK. Un score positif traduit un degré de susceptibilité à l’ectasie devant faire reconsidérer l’indication d’un LASIK
Nous avons récemment proposé de clarifier les termes utilisés pour décrire le kératocône débutant : kératocône fruste, kératocône suspect, kératocône infraclinique, etc. Nous avons contribué à faire « bouger les lignes » vis à vis des moyens permettant de dépister ces anomalies: malgré le fait que le dépistage actuel « officiel » repose sur l’utilisation de la topographie cornéenne antérieure (disque de Placido), nous avons récemment montré que les données recueillies au niveau de la face postérieure et de la pachymétrie « point par point » sont utiles pour mieux discriminer les formes les plus précoces de kératocône :
Saad A, Gatinel D. Topographic and tomographic properties of forme fruste keratoconus corneas. Invest Ophthalmol Vis Sci. 2010 Nov;51(11):5546-55. Epub 2010 Jun 16.
(article à télécharger : Topographic and Tomographic properties of FFKC Saad Gatinel IOVS ).
Keratocône : formes suspectes et frustes
Pour aider les chirurgiens au diagnostic, il existe des logiciels qui analysent les cartes topographiques de la face antérieure de la cornée. Le terme kératocône infraclinique regroupe les formes « suspectes », qui sont dépistées comme telles par les logiciels de dépistage automatisés, par l’utilisation d’indices (ex : indices de Rabinowitz, indices de Klyce Maeda) et les formes « frustes« , qui sont considérées objectivement comme « normales » par les systèmes de détection topographique « classiques », mais présentent pour un oeil expert certaines particularités.
Observée du point de vue du chirurgien de la myopie, cette distinction revêt une dimension plus pragmatique voire dichotomique (pose d’une indication de LASIK ou abstention/ ou bien recours à une technique de surface comme la PKR ?), que diagnostique (établissement d’un diagnostic différentiel entre les différentes formes de kératocône infraclinique, de dégénérescence pellucide marginale minime ou tout pathologie de type dégénératif non inflammatoire, attribution d’un grade évolutif précis, ect.. ).
Dans cette optique, les formes « suspectes » ne causent pas de souci particulier car elles sont par définition détectée par les systèmes de détection automatisés (certaines formes « suspectes » sont parfois classées comme telles par excès: les conséquences de cette erreur de classification en faux positif sont moins graves que celle d’une erreur en faux négatif. Il est donc crucial de mieux détecter les kératocônes « frustes », c’est à dire les formes les plus précoces de kératocône infra clinique.
Nous regrouperons ainsi sous l’étiquette de « kératocône fruste (infra clinique débutant) les cornées aux aspects topographiques intermédiaires entre normalité et kératocône suspect. Ce sont des cornées « à risque biomécanique pour le LASIK », qui ne présentent souvent d’après notre expérience que quelques anomalies de degré mineur (amincissement modéré, légère asymétrie). Cette approche est simplificatrice mais repose sur le fait que l’étude rétrospective de cas d’ectasie révèle la présence de ces signes souvent discrets sur les cartes topographiques préopératoires. De même, l’étude attentive de l’œil jugé comme « normal » chez des patients atteint de kératocône ^primitif dit « unilatéral » permet de déceler ce type d’anomalies.
L’identification de ces « anomalies » topographiques est donc primordiale au terme de l’évaluation préopératoire d’un patient candidat au LASIK et a fait l’objet du travail de recherche publié récemment (voir plus haut). Les résultats de notre étude prouvent qu’il faut utiliser les données issues de la face postérieure de la cornée, et les données issues de la carte d’épaisseur « point par point » (pachymétrie optique). Nos conclusions permettent d’envisager la réalisation à court terme d’un nouveau test de dépistage du kératocône fruste avec l’Orbscan, nettement plus sensible et spécifique que les logiciels actuels, en utilisant tous nos indices au sein d’une fonction discriminante.
Les patients qui présentent des anomalies topographiques évocatrices de ce que l’on appelle « kératocône fruste » avouent souvent s’être frotté régulièrement les yeux, en raison d’allergies, ou d’efforts visuels prolongés sur écran. Certains patients n’ont pas conscience de se frotter les yeux, même quand ces frottements sont vigoureux. Une forme particulière d’asymétrie de courbure avec épaisseur conservée se rencontre chez des patients qui dorment dans une position où l’oeil est « comprimé » par l’oreiller, le matelas, la main, l’avant bras, etc. Cette association est méconnue, mais elle est remarquable en clinique pour qui veut bien la rechercher.
Il est possible que le kératocône ne soit pas une maladie génétique, mais simplement un tableau clinique et topographique correspondant à des lésions mécaniques répétées des cornées. Cette hypothèse est difficile à prouver, mais aucune donnée clinique ou expérimentale ne peut non plus l’infirmer, et elle possède l’avantage d’expliquer certains « mystères » rencontrés dans l’exploration de cette pathologie.
Dans tous les cas, la présence d’anomalies topographiques traduit un état de fragilisation biomécanique et il convient de reconsidérer l’indication du LASIK dans ce genre de situation.
Caractéristiques topographiques devant faire reconsidérer l’indication d’un LASIK :
Aspects topographiques
En pratique, il faut récuser l’indication du LASIK en cas de positivité d’un ou plusieurs de ces indices classiques de détection (kératocône de forme suspecte). Cette indication ne pourra être reconsidérée qu’une fois le diagnostic différentiel effectué avec certitude (corneal warpage) et la suspicion de « cornée biomécaniquement fragile pour le LASIK » éliminé.
Aucun des « indices quantitatifs topographiques » ne possède de valeur prédictive (positive ou négative) égale à 100%. Ce manque de spécificité reflète l’importance de la déviation standard de la distribution des valeurs numériques des différents paramètres cornéens (kératométrie moyenne, valeur de l’astigmatisme cornéen, ect…). Autrement dit, pour le praticien qui ne se fonderait que sur le seul résultat de ce type d’indices, les risques respectifs d’opérer un patient atteint de kératocône fruste en cas de test pourtant négatif, ou de ne pas opérer un patient exempt de kératocône débutant en cas de test pourtant positif, ne seraient pas nuls. Le risque lié à la fausse négativité du test est évidemment beaucoup plus préjudiciable pour le patient, et la valeur prédictive négative d’un test de dépistage du kératocône revêt un caractère très important.
La négativité d’un ou plusieurs test de dépistage n’exclut donc pas avec certitude le diagnostic de kératocône fruste et le recueil et l’analyse d’éléments anamnestiques (antécédents familiaux de kératocône, terrain atopique) et cliniques (examen biomicroscopique) ainsi que l’analyse qualitative des cartes topographiques postérieures d’élévation et d’épaisseur demeurent actuellement indispensables dans ce contexte.
Randleman a proposé un score pour quantifier le risque d’ectasie ou l’âge, l’épaisseur cornéenne préopératoire, la valeur de l’épaisseur du mur postérieur, les aspects topographiques préopératoire et le degré de myopie à traiter constituent les principaux critères (21). L’intérêt de ce type de classification est contesté par certains auteurs, qui émettent des doutes quand à sa sensibilité.
La présence d’un asymétrie, qu’elle soit constatée au niveau d’une cornée (toricité asymétrique, élévation asymétrique, distribution pachymétrique asymétrique, ect..), ou entre les deux cornées (perte de la symétrie en miroir = énantiomorphisme) doit toujours faire évoquer la possibilité d’un kératocône fruste, même si les tests de dépistage classique sont négatifs.
Il est souvent utile d’utiliser les différentes échelles (individualisée, absolue) et connaître les particularités des modes de représentation topographiques (mode axial, tangentiel, gaussien…). L’algorithme de courbure tangentielle est par nature plus sensible aux rapides variations locales de courbure et possède une sensibilité supérieure à l’algorithme de courbure axiale dans ce contexte. Le diagnostic de dégénérescence pellucide marginale est facilement effectué à ce stade en reconnaissant l’aspect typique en « moustaches gauloise » de la carte topographique axiale.
Une étude destinée à définir le pas d’échelle la plus appropriée pour la détection du kératocône en topographie d’élévation a conclu à un compromis optimal entre spécificité et sensibilité égal à 10 microns d’élévation pour la face antérieure, et 20 microns pour la face postérieure de la cornée (16). Le critère de positivité retenu dans cette étude était la présence de plus de trois couleurs dans les 3 millimètres centraux. L’utilisation par défaut du mode « float » pour le calcul de la sphère de référence aboutit à une réduction de l’expression de l’asymétrie en élévation. Il peut ainsi s’avérer utile d’utiliser les modes « axis » ou « pinned » (15) qui rehaussent les différences d’élévation liées à une déformation asymétrique de la cornée.
L’existence réelle d’une ectasie limitée à la face postérieure de la cornée (terme généralement employé pour désigner une élévation centrale marquée de la face postérieure par rapport à la surface de référence calculée) a été un temps controversée, accusée d’être liée à un artéfact de reconstruction, ou une interprétation subjective des images d’élévation liée à la présence d’une asphéricité physiologique plus prolate à ce niveau. L’existence d’une élévation postérieure marquée ou de répartition globale différente de celle de la face antérieure est toutefois très souvent retrouvée en cas de kératocône fruste dans notre expérience. De fait, une élévation postérieure accrue sur le point le plus fin est un facteur utile pour discriminer le kératocône fruste ( Saad A, Gatinel D. Topographic and tomographic properties of forme fruste keratoconus corneas. Invest Ophthalmol Vis Sci. 2010 Nov;51(11):5546-55). Cet indice est un des critères retenus pour la présentation graphique du logiciel SCORE Analzer.
Nous avons publié les résultats d’une étude conduite chez des sujets qui présentaient une forme suspecte de kératocône sur l’aspect topographique en topographie spéculaire (face antérieure de la cornée), et dont les conclusions confirmaient la présence d’anomalies de la face postérieure de la cornée (17).
Le re-calcul d’une surface de référence pour la représentation de chaque examen ne permet pas de mesurer des écarts de position dans le temps avec certitude (18). Ainsi, même en l’absence d’autres anomalies, un « aspect d’ectasie postérieure » associé à une faible pachymétrie minimale est évocatrice de kératocône fruste. Cette suspicion sera renforcée par la mesure d’une asphéricité particulièrement prolate au niveau de la face antérieure (indice d’asphéricité Q inférieur à -0,10).
Un travail de modélisation informatique plublié récemment explique pourquoi en cas de kératocône débutant, l’élévation postérieure est un marqueur précoce des modifications que subit la cornée (télécharger cet article : Gatinel et al. Best Fit Sphere Elevation Asphericity Topography
En pratique , en cas de doute, il est recommandé de différer la réalisation d’une chirurgie réfractive photoablative et d’effectuer un contrôle topographique différé dans le temps. Il est alors possible de réaliser une ou plusieurs cartes différentielles dont les données sont très utiles dans ce contexte. Ces cartes pourront en effet révéler la présence de modifications topographiques évocatrices de « fragilité biomécanique » (cambrure asymétrique évolutive, amincissement, ect…)
Aspects pachymétriques (tomogaphie)
La pachymétrie optique est fiable en préopératoire, et peut être étalonnée sur la pachymétrie ultrasonique par ajustement du facteur acoustique avec l’Orbscan (19) Rappelons que la pachymétrie ultrasonique conventionnelle ne permet pas de mesurer avec certitude la valeur et la localisation de la pachymétrie minimale. En revanche, la topographie d’élévation directe par balayage permet le recueil de données utiles comme les coordonnées et la mesure pachymétrique en regard du point de plus faible épaisseur, en général situé dans le quadrant temporal inférieur. Cette localisation reste préférentielle en cas de kératocône avéré ou fruste, mais son excentricité (sa distance au centre de la cornée) est statistiquement plus importante dans cette pathologie (19) (voir Figure 1). Le recueil de la valeur et des coordonnées de la pachymétrie minimale est par ailleurs utile pour le calcul théorique de l’épaisseur cornéenne résiduelle après LASIK. Surtout, le gradient d’amincissement vers le centre est accru en cas de kératocône fruste, indépendamment de la valeur de l’épaisseur minimale. Même si une épaisseur cornéenne moindre que la moyenne (ex : inférieure à 500 microns) est plus fréquente en cas de kératocône infra clinique, c’est surtout l’existence d’un amincissement plus rapide vers le centre de la cornée (différence accrue entre l’épaisseur périphérique et centrale).
Signes cliniques associés au risque d’ectasie
L’âge et le terrain allergique constituent des facteurs de risque pour la présence d’une forme infra-clinique de kératocône. Plus un patient est jeune, plus la probabilité d’être confrontée à une forme latente de kératocône est importante. La notion de frottements oculaires répétés est également péjorative ( et pourrait être incriminée dans la genèse des anomalies topographiques comme l’asymétrie ou l’amincissement cornéen).
La place des indices de dépistage topographique du kératocône
La vidéotopographie spéculaire est limitée à l’étude de la courbure de la face antérieure de la cornée mais bénéficie d’une ancienneté supérieure à la topographie d’élévation. Les premiers indices proposés pour la détection du kératocône sont issus des données de courbure (indice de Klyce-Maeda, indice de Rabinowitz, ect…). Ils dérivent du croisement de données de courbure recueillies sur de larges échantillons et d’algorithmes de détection (intelligence artificielle). Ces indices ont fait l’objet de publications scientifiques validées (Klyce Maeda, ect) (20).
D’autres indices ont été par la suite proposés à partir des données d’élévation fournies par l’Orbscan (critères de Rousch, calcul du rapport entre le rayon des sphères de références respectives de la face antérieure et postérieure de la cornée,ect…) mais ils n’ont fait l’objet d’aucune étude publiée ni d’évaluation précise de leur sensiblilité et spécificité. Nous avons finalement démontré que ces données avaient une utilité pour dépister avec une sensibilité et une spécificité accrue les formes frustes de kératocône: Topographic and Tomographic properties of FFKC Saad Gatinel IOVS.
Un nouveau test de dépistage découlant des résultats de ce travail est en cours de réalisation.
En pratique… comment prévenir le risque d’ectasie cornéenne?
Quand la cornée est d’épaisseur normale et sans anomalies topographiques (absence de signes de kératocône fruste), mais que l’amétropie du patient implique une profondeur d’ablation importante, la découpe d’un volet fin est recommandée afin de réduire le risque de violation du mur postérieur. Si l’amétropie est trop importante par rapport à l’épaisseur de cornée initiale, une abstention, ou une technique non cornéenne peut être proposée (implant phake, ou pseudophake selon l’âge, l’état du segment antérieur,etc…).
Notre expérience confrontée à l’étude exhaustive des cas publiés dans la littérature nous incite actuellement à récuser pour le LASIK (en plus des contre-indications classiques pour cette indication comme le kératocône avéré ou fruste identifié) les candidats à une chirurgie réfractive présentant un ou plusieurs des signes suivants, même si les indices de détection automatisés du kératocône sont négatifs (pas de suspicion):
-un astigmatisme topographique asymétrique ou irrégulier même modéré, en particulier si son axe est oblique ou inverse, non ou faiblement corrélé à l’axe de l’œil adelphe (faible énantiomorphisme) et si la pachymétrie optique ou ultrasonique centrale moyenne est inférieure à 510 microns.
-une pachymétrie centrale moyenne inférieure à 500 microns et/ou une pachymétrie minimale inférieure à 500 microns, quelque soient l’aspect topographique et la valeur prédite par le calcul prédictif de l’épaisseur résiduelle du mur postérieur.
-une perte de l’énantiomorphisme marquée (perte de l’aspect de symétrie en miroir entre les deux yeux), sans antécédents cornéens traumatiques ou infectieux.
-une excentricité accrue vers la direction temporale inférieure du point le plus fin.
-une élévation accrue (supérieure à 25 microns) de la face postérieure vis à vis de la sphère de référence calculée.
Le logiciel SCORE Analyzer a été conçu pour recueillir de manière automatisée ce type d’anomalies topographiques et calculer un score permettant de situer de manière objective la cornée étudiée (topographe Orbscan). Quand ce score est positif, l’indication de LASIK doit être revue.
Ces recommandations sont issues de notre expérience et leur validité a en partie été démontrée. Une attitude pragmatique dictée par la prudence et destinée à réduire au maximum le risque d’opérer un patient atteint de kératocône fruste non détecté ou d’une « cornée à risque biomécanique » pour le LASIK. Dans ce contexte, il vaut mieux récuser qu’inclure par excès !
Les patients récusés pour le LASIK peuvent être réorientés selon les cas en contactologie, ou vers une chirurgie additive (implant, anneaux, ect…) ou photoablative de surface (PKR, LASEK),en particulier si la profondeur d’ablation programmée est modérée (inférieure à 70 ou 80 microns). La technique de surface doit être effectuée de façon soigneuse afin de permettre réduire le risque de haze pour les profondes ablations de surface.
La réalisation d’un traitement personnalisé de surface guidé par la topographie est particulièrement indiquée en cas d’astigmatisme réfractif irrégulier d’origine cornéenne (augmentation du taux des aberrations optiques de haut degré) (22). Les résultats publiés dans la littérature concernant le devenir des patients atteints de kératocône fruste avec réfraction stabilisée opérés en PKR sont satisfaisants et ne révèlent pas une influence péjorative de cette technique sur l’évolution du kératocône fruste (23,24). Récemment, la survenue d’une ectasie a été rapportée 22 mois après réalisation d’un LASIK sur l’œil gauche d’un patient myope dont l’épaisseur cornéenne centrale était de 500 microns et l’aspect topographique marqué par l’existence d’un astigmatisme asymétrique. Alors qu’il présentait une cornée plus fine (485 microns), un aspect topographique et une myopie équivalente, l’œil droit qui avait été opéré en PKR au même moment n’a pas développé d’ectasie (25).
La PKR fait-elle courir un risque d’ectasie chez les patients atteints de formes suspectes de kératocône ?
Cette question découle du fait que la PKR (technique de surface sans capot) comporte une étape de photoablation et représente donc un risque potentiel d’affaiblissement cornéen. Le nombre de cas d’ectasie après technique de surface est faible, et leur analyse révèle pratiquement à chaque fois la présence d’une forme certes débutante mais avérée de kératocône (encore plus rarement la présence d’une forme suspecte ou infraclinique), qui aurait pu de toutes façons évoluer sans réalisation de la photoablation.
A l’inverse, il existe des séries publiées de photoablation de surface chez des sujets présentant des cornées suspectes qui ne montrent pas d’effet péjoratif de cette technique.
Un raisonnement simple permet d’ailleurs de réfuter la nocivité des techniques de surface pour les formes suspectes. La PKR est une technique plus ancienne que le LASIK, et qui a donc été réalisée chez de nombreux patients présentant des cornées suspectes (quoique non identifiées comme telle à l’époque car la réalisation d’une topographie n’était pas systématique avant chirurgie, et les critères de dépistage du kératocône plus permissifs). De plus, les magnitudes des traitements délivrés étaient plus importantes qu’aujourd’hui. Enfin, il n’y avait pas de précautions particulières vis à vis de la prévention d’une ectasie, car cette complication ne fut décrite… qu’en 1998, soit au début de la période d’essor du LASIK. Ainsi, si la PKR accentuait significativement le risque d’évolution vers l’ectasie, alors il devrait exister autant voire beaucoup plus de cas de kératocônes iatrogène post-PKR que post-LASIK !
Le cross linking est il conseillé après ectasie?
L’auteur de ce site ne considère pas que le cross linking a prouvé son efficacité en matière de restauration ou amélioration même partielle de la biomécanique cornéenne. Une page est consacrée aux raisons de ce scepticisme. Aucune étude n’a montré que la résistance biomécanique cornéenne augmentait in vivo après cross linking (CXL), malgré l’utilisation de divers instruments (Ocular Response Analyzer, CorVIS, etc.). Les modifications observées après cross linking sont très probablement liées à des modifications épithéliales cicatricielles, et la délivrance d’une irradiation UV sur une cornée déjà fragilisée par le LASIK et l’ectasie ne parait pas souhaitable. Aucune ectasie n’a régressé spontanément, ni après cross linking. Une stabilisation de la topographie cornéenne peut être obtenue si le patient arrête de se frotter les yeux, et que la pression intra oculaire est maîtrisée. De plus, des cas de « haze » ont été observés après cross linking pour ectasie… sans réduction aucune de l’ectasie.
La prescription d’un CXL en présence d’une ectasie cornéenne induite par la chirurgie est souvent justifiée comme une mesure destinée à ralentir l’ectasie. Le CXL est même parfois préconisé du côté de l’oeil non atteint en cas d’ectasie unilatérale. Etant donné l’absence de preuve clinique de l’efficacité de cette technique, et l’évidence qu’elle échoue à induire un durcissement mesurable de la rigidité cornéenne, il semble logique d’expliquer au patient qu’il ne faut pas (plus) se frotter les yeux, et s’astreindre à une surveillance topographique rapprochée. Le CXL est une technique qui induit un stress oxydatif majeur du mur cornéen, et au décours d’une chirurgie réfractive, le risque d’inflammation du tissu cornéen stromal est important (haze).
Dans l’exemple suivant, la réalisation d’un crosslinking bilatéral après ectasie unilatérale n’a pas modifié significativement les valeurs des paramètres biomécaniques mesurés par l’Ocular Response Analyzer (ORA). En revanche, il a entrainé un haze bilatéral avec réduction de la vision et gêne en forte luminosité pendant plusieurs mois.
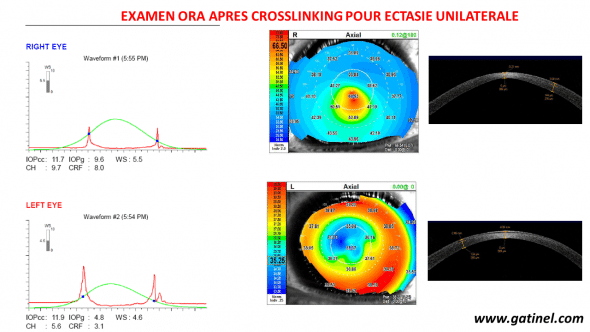
Makgré la réalisation d’un CXL, aucune amélioration de la rigidité cornéenne n’est mesurée, ni du côté de l’ectasie, ni du côté sans ectasie.
Conclusion : LASIK et risque d’ectasie
Le LASIK est l’acte de chirurgie réfractive le plus pratiquée pour la correction des amétropies sphéro-cylindrique. Outre son confort, cette suprématie reflète l’ importante sécurité et prédictiblité de cette technique, acquises au fil du temps grâce à l’expérience croissante des chirurgiens et les améliorations successives des matériels dévolus à la découpe du volet stromal (laser femtoseconde, microkératomes de nouvelle génération) et à la délivrance de la photoablation. Ainsi, la plupart des complications per ou post opératoires peuvent aujourd’hui être prévenue par une sélection rigoureuse des patients ou la mise en œuvre de mesures prophylactiques et thérapeutiques adaptées.
La réalisation d’une technique de surface est préférable en cas de doute clinique, car il n’existe pas d’arguments fondés en faveur du caractère iatrogène de cette technique vis à vis des cornées suspectes. Les résultats fonctionnels attendus sont identiques à ceux du LASIK réalisé chez des sujets dont les cornées sont normales.
L’ectasie cornéenne induite ne doit pas déroger à cette évolution et son incidence devrait être réduite au minimum par le strict respect des règles et principes abordés dans cet article.
Résumé / Points clés
La réalisation de volets fins (90 à 110 microns environ) est recommandée pour réduire les risques d’ectasie chez les forts myopes opérés en LASIK.
La simple réalisation d’un volet cornéen (sans photoablation) effectuée sur une cornée fragile sur le plan biomécanique (kératocône fruste) peut conduire à l’apparition d’une ectasie cornéenne progressive.
Une suspicion de kératocône fruste doit faire reconsidérer l’indication de LASIK. Sa confirmation ou l’absence d’élimination formelle de ce diagnostic contre-indique la réalisation d’un LASIK.
Il n’existe pas de test de sensibilité et de spécificité absolues pour le dépistage des formes frustes de kératocône: certaines stratégies, incluant un nombre important d’indices permettent d’accroître la sensibilité et la spécificité du dépistage.
Un test de dépistage topographique négatif, en particulier quand il se limite à l’étude de la seule face antérieure de la cornée n’exclut pas formellement la présence d’une forme fruste de kératocône dont l’évolution pourrait s’accélérer après LASIK.
L’asymétrie entre les deux cornées (perte de l’énantiomorphisme), l’astigmatisme asymétrique ou irrégulier associé à une cornée fine (épaisseur moyenne centrale inférieure à 510 microns, épaisseur minimale inférieure à 500 microns, amincissement rapide vers un point le plus fin situé en temporal inférieur) doivent faire reconsidérer l’indication du LASIK. En cas de doute, il est préférable d’opter pour une technique sans découpe lamellaire (technique de surface, implant, insertion d’anneau intra-cornéen, ect…en fonction de l’amétropie du patient).
Références
1) Binder PS. Ectasia after laser in situ keratomileusis. J Cataract Refract Surg,2003;29:2419-2429
2) Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD.Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology,2003;110(2):267-75
3) Comaish IF, Lawless MA. Progressive post-LASIK keratectasia: biomechanical instability or chronic disease process? J Cataract Refract Surg,2002;28(12):2206-13.
4) Seitz B, Rozsival P, Feuermannova A, Langenbucher A, Naumann GO. Penetrating keratoplasty for iatrogenic keratoconus after repeat laser in situ keratomileusis : histologic findings and litterature review. J Cataract Refract Surg, 2003;29(11):2217-24
5) O’donnell C, Welham L, Doyle S. Contact lens management of keratectasia after laser in situ keratomileusis for myopia. Eye Contact Lens, 2004;30(3):144-6
6) Choi HJ, Kim MK, Lee JL. Optimization of contact lens fitting in keratectasia patients after laser in situ keratomileusis. J Cataract Refract Surg, 2004;30(5):1057-66
7) Colin J, Velou S. Implantation of Intacs and a refractive intra-ocular lens to correct keratoconus. J Cataract Refract Surg,2004;29(4):832-4
8) Pokroy R, Levinger S; Hirsh A. Single Intacs segment for post-laser in situ keratomileusis keratectasia. J Cataract Refract Surg,2004;30(8):1685-95
9) Seo KY, Lee JH, Kim MJ, Park JW, Chung ES, Lee YS, Kim EK. Effect of suturing on iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg,2004;20(1):40-5
10) Faraj HG, Gatinel D, Chastang PJ, Hoang-Xuan T.Corneal ectasia after LASIK. J Cataract Refract Surg, 2003;29(1):220.
11) Flanagan GW, Binder PS. Precision of flap measurements for laser in situ keratomileusis in 4428 eyes.J Refract Surg,2003;19(2):113-23.
12) Giledi O, Daya SM. Unexpected flap thickness in laser in situ keratomileusis. J Cataract Refract Surg,2003;29(9):1825-6.
13) Haw WW, Manche EE. Iatrogenic keratectasia after a deep primary keratotomy during laser in situ keratomileusis. Am J Ophthalmol. 2001;132(6):920-1.
14) Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg 2001;27(11):1796-802.
15) Faraj H, Gatinel D. Ectasie cornéenne induite par le LASIK. In Gatinel D, Hoang-Xuan T « Le LASIK : de la théorie à la pratique », Elsevier, 2003, pp356-363, Paris
16) Tanabe T, Oshika T, Tomidokoro A, Amano S, Tanaka S, Kuroda T, Maeda N, Tokunaga T, Miyata K.Standardized color-coded scales for anterior and posterior elevation maps of scanning slit corneal topography. Ophthalmology, 2002;109(7):1298-302.
17) Schlegel Z, Hoang-Xuan T, Gatinel D. Comparison of and correlation between anterior and posterior corneal elevation maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg. 2008;34(5):789-95.
18) Yoshida T, Miyata K, Tokunaga T, Tanabe T, Oshika T.Difference map or single elevation map in the evaluation of corneal forward shift after LASIK. Ophthalmology, 2003;110(10):1926-30.
19) Prisant O, Calderon N, Chastang P, Gatinel D, Hoang-Xuan T. Reliability of pachymetric measurements using orbscan after excimer refractive surgery. Ophthalmology. 2003;110(3):511-5.
20) Rabinowitz YS, Rasheed K. KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg, 1999;25(10):1327-35.
21) Randleman JB, Trattler WB, Stulting RD. Validation of the Ectasia Risk Score System for preoperative laser in situ keratomileusis screening. Am J Ophthalmol. 2008;145(5):813-8.
21) Dausch D, Scroder E, Dausch S. Topography-controlled excimer laser photorefractive keratectomy. J Refract Surg, 2000;16(1):13-22
22) Kasparova EA, Kasparov AA. Six-year experience with excimer laser surgery for primary keratoconus in Russia. J Refract Surg,2003;19:S250-4
23) Bilgihan K, Ozdek SC, Konuc O, Akata F, Hasanreisoglu B. Results of photorefractive keratectomy in keratoconus suspects at 4 years. J Refract Surg, 2000;16(4):438-43
24) Rao SK, Srinivasan B, Sitalakshmi G, Padmanabhan P. Photorefractive keratectomy versus laser in situ keratomileusis to prevent keratectasia after corneal ablation. J Cataract Refract Surg, 2004;30:2623-8

Je pourrai vous recevoir à la Fondation Rothschild si vous le souhaitez, en attendant il est crucial de cesser tout frottement des deux côté et vérifier que votre position de sommeil n’induit pas une compression ou un appui oculaire prolongé du côté gauche. Si vous cessez les frottements, l’ectasie ne progressera pas – et inversement!
Bonjour Docteur Gatinel,
J ai fait le lasik en 2018.
Rapidement j au remarqué que je voyais double de l’oeil gauche. A ce jour on me confirme une ectasie et on me propose la technique de crosslicking. J ai lu votre article sur cette technique qui d apres vous n a pas fait ses preuves.
Que ne conseillez vous de faire pour une ectasie post lasik ?
J avais obtenu une consultation a l institut rotschild et une ordonnance pour votre service mais je n’ai jamais réussi à prendre rdv.
L intervention, si elle se confirme, doit avoir lieu en Juin 2022. J ai récupéré mon dossier médical avec les topographie avant et après lasik. J’aimerai vraiment pouvoir avoir votre regard.
Dans mon expérience, l’ectasie post LASIK survient chez des patients dont les frottements avaient déjà fragilisé la cornée avant l’intervention, mais sans que les manifestations topographiques de la déformation n’aient été identifiés par le chirurgien. La poursuite des frottements après le LASIK (sécheresse oculaire) aggrave le tableau car la cornée étant amincie, ceci favorise la poursuite de la déformation. Cette vision est étayée par le fait que l’arrêt des frottements (et la modification de la position de sommeil accessoirement si elle implique l’oeil avec l’ectasie) suffit pour enrayer la déformation cornéenne. Ceci rend le CXL inutile: l’indication de la greffe est justifiée quand il n’est plus possible de corriger la vision par des lunettes, des lentilles, etc. Il existe des risques liés au CXL comme l’induction d’une inflammation, d’un retard cicatriciel de l’épithélium, un haze, une infection, etc. Les chirurgiens poussent souvent à cette indication car ils redoutent bien entendu une évolution de l’ectasie pour son propre compte, alors que si l’on en comprend le mécanisme primitif, ceci ne risque de survenir qu’en cas de poursuite des contraintes mécaniques sur le dôme cornéen. Arrêtez celles-ci complètement (frottements liés au démaquillage inclus) et effectuez des topographies cornéennes différentielles, qui sont un moyen objectif de suivre avec précision l’état de la cornée.
Merci infiniment pour cet article compréhensible même pour les non-professionnels.
Je suis atteinte d’une extasie post lasik mais j’ai deux avis médicaux: l’un me suggère fortement un cross-linking, l’autre ayant détecté un début de cataracte me propose plutôt une opération de celle-ci et l’implant d’une lentille qui diminuerait le kératocône par aplatissement. J’ai par ailleurs lu que le cross-linking est irréversible et serait un prélude à une greffe de la cornée. Que décider? pourrais-je continuer à vivre sans intervention et me contenter de ne pas me frotter l’oeil et hydrater continuellement?
[…] Ectasie Cornéenne […]
[…] Ectasie Cornéenne […]